Lung cancer remains one of the most formidable challenges in contemporary oncology, with invasive mucinous adenocarcinoma representing a particularly aggressive variant of this disease. In a recent multicenter study authored by Zheng et al., significant advancements have been made in understanding lymph node metastasis in patients diagnosed with resectable lung invasive mucinous adenocarcinoma. This research not only sheds light on metastatic patterns but also proposes an optimal lymph node dissection strategy aimed at improving surgical outcomes for this patient demographic.
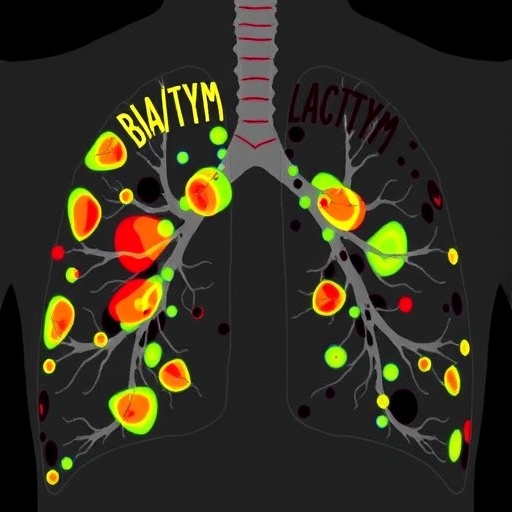
The intricacies of lymph node involvement in lung cancer are of paramount importance to clinicians and researchers alike. Identifying the lymph node metastasis atlas created in this study offers groundbreaking insights into how and where this cancer type commonly spreads. The atlas serves as a vital tool, as it underscores the specific lymphatic pathways often traversed by metastatic cells, thereby allowing surgeons to map out their approach to lymph node dissection more effectively.
By examining a large cohort of patients from multiple institutions, Zheng and his colleagues have built a robust dataset that reflects real-world outcomes. This diversity in the patient population strengthens the validity of their findings and provides a clearer picture of how invasive mucinous adenocarcinoma behaves across different demographics and clinical settings. This type of research is critical as it not only enriches the academic literature but also translates into practical strategies that can enhance patient care.
Crucial to the authors’ methodology was the use of advanced imaging techniques and histopathological analysis. These modalities were instrumental in accurately identifying metastatic lymph nodes and determining their status concerning the primary tumor. The strength of their investigative approach lies in its comprehensiveness; every aspect, from the preoperative imaging studies to postoperative histology, was meticulously documented, laying the groundwork for a thorough analysis.
Another significant aspect of this study is its focus on optimal lymph node dissection strategies. The findings suggest a tailored approach, emphasizing the need for personalized surgical interventions based on the individual metastatic patterns outlined in the lymph node metastasis atlas. This adaptability could lead to more refined surgical techniques that minimize morbidity while maximizing oncological clearance, thereby potentially improving overall survival rates.
Moreover, the discussion around the clinical implications of these findings cannot be understated. As the study progresses to outline practical recommendations, it paves the way for standardizing lymph node dissection practices, which have historically varied widely among surgical oncologists. By advocating for a more uniform approach, clinicians can optimize surgical pathways that are backed by evidence-based strategies derived from a thorough understanding of the disease itself.
Listening to the voices of patients involved in this study further emphasizes the urgency and importance of the findings. Many patients undergoing treatment for lung invasive mucinous adenocarcinoma struggle not just with the disease but also with the complex surgical decisions that follow their diagnosis. By providing a clearer trajectory for lymph node management, this research engenders hope for improved clinical decisions that can directly impact patient outcomes.
In addition, the implications for future research cannot be overlooked. The establishment of this lymph node metastasis atlas not only serves current clinical needs but also opens avenues for further studies into the molecular mechanisms underpinning the metastatic process itself. Understanding the biological behavior of lung invasive mucinous adenocarcinoma may lead to the identification of novel therapeutic targets and intervention strategies.
As the landscape of lung cancer treatment evolves, incorporating findings from studies like that of Zheng et al. will be crucial. It challenges the status quo of oncological approaches, urging practitioners to adapt their methodologies as new evidence emerges. This commitment to continual learning and adaptation highlights the dynamic nature of cancer treatment paradigms and the necessity for oncologists to remain vigilant.
The authors’ contribution to the field extends beyond mere numbers and statistical analyses; they have provided an essential reference point for future clinical trials and interventions focused on lung cancer. Their work encourages collaboration among various oncology disciplines, fostering a multidisciplinary approach aimed at tackling the complexities of cancer management.
As the medical community continues to unravel the complexities of invasive mucinous adenocarcinoma, studies like these are essential building blocks that keep the momentum of innovation alive. They remind us that behind each statistic is a patient’s journey, underscoring the profound impact that targeted, evidence-based strategies can have on individual lives.
For healthcare providers, this research translates complex data into actionable insights, fostering better decision-making processes that prioritize patient quality of life and longevity. The shift toward a more precise, data-informed approach signifies not only an advancement in surgical oncology but also a commitment to enhancing patient experiences and outcomes in the face of challenging diagnoses.
In conclusion, Zheng and his team’s breakthrough in mapping lymph node metastasis and optimizing dissection strategies for patients with resectable lung invasive mucinous adenocarcinoma represents a substantial advancement in the field of oncology. Their work encapsulates the essence of clinical research — a continuous cycle of understanding, innovation, and patient-centered care that ultimately strives to conquer one of the leading causes of cancer-related deaths worldwide.
Subject of Research: Lung invasive mucinous adenocarcinoma and lymph node metastasis.
Article Title: Identification of the lymph node metastasis atlas and optimal lymph node dissection strategy in patients with resectable lung invasive mucinous adenocarcinoma: a real-world multicenter study.
Article References:
Zheng, C., Zhang, GC., Zhang, L. et al. Identification of the lymph node metastasis atlas and optimal lymph node dissection strategy in patients with resectable lung invasive mucinous adenocarcinoma: a real-world multicenter study. Military Med Res 12, 67 (2025). https://doi.org/10.1186/s40779-025-00659-3
Image Credits: AI Generated
DOI:
Keywords: Lung cancer, invasive mucinous adenocarcinoma, lymph node metastasis, lymph node dissection, oncological surgery, clinical study, patient outcomes.