Lip and oral cavity cancer (LOCC) has emerged as a critical global health concern, marked by escalating incidence, mortality, and disability-adjusted life-years (DALYs) across diverse populations. Despite ongoing advances in medical technology and preventive measures, the disease continues to impose a disproportionate burden on low- and middle-income regions, exposing persistent health disparities worldwide. A recent comprehensive and methodologically robust study has analyzed trends in LOCC from 1990 to 2021 and employed sophisticated forecasting to project disease trajectories through 2036, highlighting stark regional differences and the influence of major risk factors.
Leveraging the extensive data repository of the Global Burden of Disease Study (GBD) 2021, researchers undertook a granular evaluation of LOCC’s global, regional, and national epidemiology. The analysis encompassed crucial metrics, including incidence rates, mortality figures, and DALYs, providing an integrated measure of both premature death and disability attributable to LOCC. Notably, this research utilized the Bayesian Age-Period-Cohort (BAPC) model to generate forward-looking projections, a state-of-the-art statistical approach that accounts for temporal changes across different age groups, calendar periods, and birth cohorts.
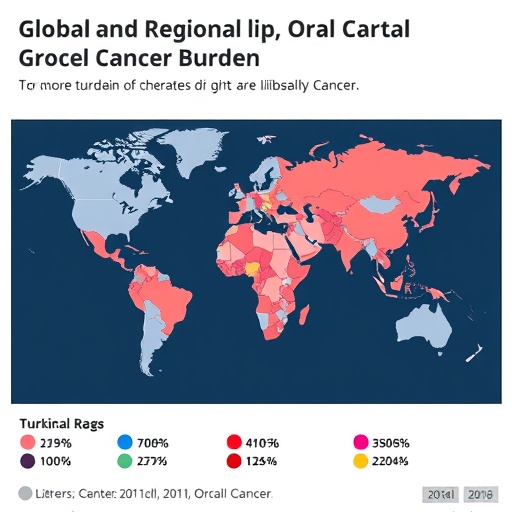
The study’s findings reveal sobering trends and underscore the urgent need for targeted public health interventions. Globally, the number of new LOCC cases in 2021 surpassed 420,000, with South Asia bearing the highest burden. This region exhibited an age-standardized incidence rate of 9.8 per 100,000, far exceeding global averages. The mortality rate associated with LOCC demonstrated a striking increase of nearly 114% since 1990, culminating in over 208,000 deaths in 2021 alone. This dramatic rise spotlights LOCC as a growing threat in many parts of the world, particularly where healthcare infrastructure and cancer awareness remain inadequate.
Disability due to LOCC also emerged as a major challenge, with the disease accounting for over 5.8 million DALYs in 2021, reflecting years lived with illness alongside premature mortality. Critically, the burden was disproportionately higher in low and low-middle Socio-Demographic Index (SDI) countries, underlining the intersection of poverty, limited healthcare access, and higher exposure to risk factors. The regional and socio-economic disparities accentuate the compounding effect of social determinants on cancer outcomes.
The study’s analysis of risk factor attribution further elucidates the complex etiological landscape of LOCC. Smoking was identified as the single largest contributor to mortality, accounting for 23.4% of deaths. Alcohol consumption and chewing tobacco followed closely, responsible for 19.2% and 18.7% of mortality, respectively. These findings reflect the persistence of high-risk behaviors in various populations, many of which are preventable through effective public health policies and education.
Gender-specific analysis revealed disconcerting trends, with projections indicating that females will experience a sustained rise in both LOCC incidence and associated disability. This represents a critical shift in disease epidemiology that demands tailored interventions addressing the unique vulnerabilities and exposure patterns in women. The increasing female burden highlights the imperative to expand focused screening and prevention programs beyond traditional male-dominated risk assessments.
Model-based projections to 2036 offer a nuanced perspective on the evolving LOCC landscape. While mortality rates are forecasted to decline globally, the anticipated rise in incidence and DALYs, especially among women, suggests that improved survival outcomes have not yet translated into a reduction in disease occurrence or disability. This dichotomy signals advancements in treatment efficacy but also underscores persistent challenges in early detection and primary prevention.
The study’s comprehensive approach, integrating multi-dimensional data with advanced predictive modeling, sheds light on the multifaceted burden LOCC places on health systems worldwide. These insights suggest that addressing the disease’s trajectory requires a multi-pronged strategy, combining risk factor modification, early diagnosis, and equitable healthcare delivery. The disproportionate impact on lower SDI regions calls for global solidarity and investment in underserved populations to close the gap in cancer care outcomes.
Importantly, the research serves as a call to action for public health authorities and policymakers. Without concerted efforts to reduce tobacco and alcohol use and curb risky behaviors such as chewing tobacco, the projected incidence rates could overwhelm health infrastructures, especially in South Asia and similar high-risk zones. Strengthening regulation, community education, and access to cessation programs emerges as pivotal in reversing these alarming trends.
Moreover, improvements in early detection modalities can substantially alter LOCC prognosis and reduce the disability burden. Screening programs targeting high-risk groups and enhanced training for healthcare providers in recognizing early oral lesions could facilitate timely interventions, thereby mitigating progression to advanced disease stages associated with higher morbidity and mortality.
The social and economic implications of the escalating LOCC burden are profound. Beyond the human toll, increased disease prevalence strains health budgets and workforce productivity in affected regions. This underscores the importance of integrating LOCC prevention within broader non-communicable disease strategies, emphasizing sustainable health promotion and resource allocation.
As the study highlights, the interplay between behavioral risk factors and socio-economic determinants necessitates a comprehensive public health framework, tailored to the socio-cultural contexts of diverse populations. Collaborative efforts involving governments, healthcare systems, and communities are essential to design culturally sensitive interventions that effectively reduce exposure to LOCC risk factors.
In conclusion, the escalating global burden of lip and oral cavity cancer as delineated in this rigorous analysis is a clarion call to intensify global cancer control measures. The persistent high incidence, rising mortality, and substantial disability attributed to this disease underscore the urgent need for preventive policies, early detection enhancements, and addressing social inequities. By harnessing epidemiological insights and predictive analytics, the global health community can formulate evidence-based strategies to curb the LOCC epidemic and improve outcomes for vulnerable populations worldwide.
Subject of Research: Epidemiology and future projections of lip and oral cavity cancer burden globally, regionally, and nationally, with emphasis on risk factor attribution.
Article Title: Global, regional, and national burden of lip and oral cavity cancer and projections to 2036
Article References:
Meng, S., Lv, A., Li, N. et al. Global, regional, and national burden of lip and oral cavity cancer and projections to 2036. BMC Cancer 25, 1573 (2025). https://doi.org/10.1186/s12885-025-14995-z
Image Credits: Scienmag.com