In an illuminating new study published in Nature Communications, researchers report groundbreaking insights into the immune responses against COVID-19 among people living with HIV. The work, emerging from the CoVPN 3008 study, identifies neutralizing and binding antibodies as critical correlates of protection in this particularly vulnerable population. These findings not only deepen our understanding of how immune defenses operate in the context of co-infections but also hold profound implications for tailoring vaccination and treatment strategies for immunocompromised individuals.
The global battle against COVID-19 has revealed stark disparities in disease outcomes among different populations. Among those disproportionately affected are individuals living with HIV, whose immune systems are frequently compromised due to the virus and its treatment regimens. Understanding how these individuals respond to SARS-CoV-2 infection or vaccination is indispensable for controlling the pandemic within this subgroup. The study led by Mkhize, Zhang, Brackett, and their collaborators delves into the immunological underpinnings that dictate susceptibility and resilience in people with HIV.
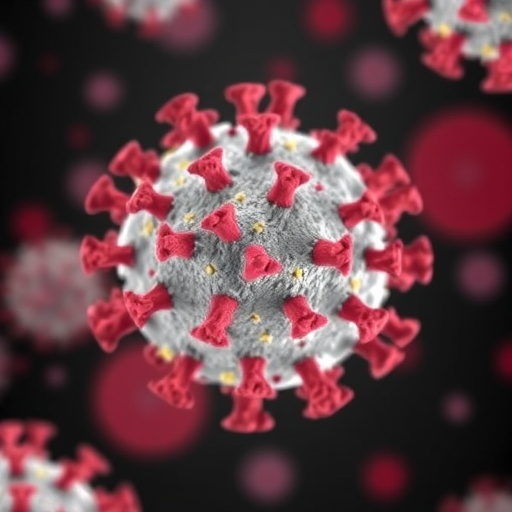
Central to the team’s investigation was an evaluation of antibody responses, specifically neutralizing and binding antibodies, which serve as defenders by either directly inhibiting viral entry into host cells or facilitating immune recognition and clearance. Neutralizing antibodies block the virus from infecting cells effectively, while binding antibodies mark the virus for destruction by other components of the immune system. The researchers sought to determine whether levels of these antibody types correlate with the risk of developing symptomatic COVID-19 in the studied population.
The CoVPN 3008 study enrolled a substantial cohort of people with HIV, carefully monitoring their antibody profiles and clinical outcomes over time. Through longitudinal sampling and rigorous serological assays, the investigators obtained comprehensive data mapping the dynamics of SARS-CoV-2-specific immune responses. Using advanced neutralization tests, they quantified the antibodies’ ability to prevent viral infection in vitro, while binding antibody levels were measured using sensitive immunoassays capable of detecting diverse epitope interactions.
Their data revealed a compelling link: higher titers of neutralizing antibodies corresponded with a markedly reduced risk of symptomatic COVID-19. Similarly, elevated binding antibody levels also conferred protection, suggesting that a robust humoral immune response is a critical shield against severe illness. These correlations persisted even after adjusting for demographic variables, HIV disease status, and antiretroviral therapy regimens, underscoring their robustness and biological relevance.
The implications of this work ripple across clinical and public health domains. It suggests that vaccine strategies for people with HIV must prioritize eliciting strong neutralizing and binding antibody responses, potentially guiding booster recommendations or novel vaccine formulations optimized for immunocompromised hosts. Moreover, these serological markers might serve as valuable surrogates in clinical trials seeking to establish correlates of protection, streamlining vaccine evaluation in vulnerable groups.
Intriguingly, the study also touches on the complex interplay between HIV-induced immune dysregulation and SARS-CoV-2 pathogenesis. While HIV compromises cell-mediated immunity, the preservation of humoral function, as indicated by these antibody responses, appears critical for defense against COVID-19. This nuanced immune landscape warrants further exploration to optimize therapeutic interventions and improve survival outcomes.
From a technical standpoint, the study employed multiplex bead-based assays for high-throughput binding antibody quantification and pseudovirus neutralization assays to model viral inhibition safely. This dual-pronged approach allowed for a granular understanding of the antibody landscape, capturing both functional neutralization and broader humoral engagement. The researchers also stratified participants by viral load and CD4+ T-cell counts, revealing that immune restoration via ART enhances antibody-mediated protection.
This research adds a pivotal piece to the evolving puzzle of COVID-19 immunology, particularly within the context of immunosuppression. By pinpointing neutralizing and binding antibodies as correlates of protection in people with HIV, the investigators provide a roadmap for future studies focused on optimizing immune responses against emerging SARS-CoV-2 variants, which may challenge current vaccine efficacy.
Furthermore, these findings may extend beyond HIV-positive populations, prompting comparative analyses across other immunocompromised cohorts such as transplant recipients or cancer patients. Understanding the shared and unique features of humoral immunity in these groups is paramount as we refine targeted interventions and anticipate the trajectory of the pandemic.
The work also underscores the pivotal role of large, well-characterized cohorts like CoVPN 3008 in generating high-quality data that bridge bench research with clinical application. Through meticulous design and longitudinal follow-up, such studies unravel immune correlates with direct relevance to patient care, moving us closer to personalized medicine in infectious diseases.
Looking ahead, the authors advocate for integrating humoral immune monitoring into routine clinical practice for people with HIV, particularly in settings where vaccine response heterogeneity remains a concern. This approach can identify individuals at heightened risk and guide timely administration of prophylactic therapies such as monoclonal antibodies or additional vaccine doses.
Moreover, the study sets the stage for exploring the durability of antibody responses post-vaccination or natural infection in people with HIV. Understanding the kinetics of antibody waning and memory B-cell formation will inform sustained protection strategies, acknowledging the potential for viral immune escape mechanisms.
In summation, this landmark investigation offers critical insight into the immunological armor that safeguards people living with HIV against COVID-19. By delineating neutralizing and binding antibodies as correlates of risk, the study delivers a message of hope grounded in scientific rigor: tailored immunological interventions can enhance disease defense even in immunocompromised populations.
As the global community confronts ongoing challenges posed by SARS-CoV-2 variants and vaccine equity issues, such research underscores the necessity of inclusive studies addressing diverse immune landscapes. The integration of immunological nuance into public health strategies promises to elevate our collective efforts in pandemic mitigation.
Ultimately, this research exemplifies the power of interdisciplinary collaboration, marrying clinical insight with cutting-edge immunology to illuminate pathways toward safeguarding all populations against infectious threats. The findings herald a new chapter in precision vaccinology, where understanding individual and group-specific immune parameters will optimize global health outcomes.
Subject of Research: Immune correlates of protection against COVID-19 in people living with HIV.
Article Title: Neutralizing and binding antibodies are a correlate of risk of COVID-19 in the CoVPN 3008 study in people with HIV.
Article References:
Mkhize, N.N., Zhang, B., Brackett, C. et al. Neutralizing and binding antibodies are a correlate of risk of COVID-19 in the CoVPN 3008 study in people with HIV. Nat Commun 16, 8876 (2025). https://doi.org/10.1038/s41467-025-63948-4
Image Credits: AI Generated