Synovial sarcoma (SS) remains one of the most enigmatic and aggressive malignant mesenchymal neoplasms, notable for its unusual capacity to exhibit variable epithelial differentiation. Affecting predominantly young adults, this tumor challenges clinicians and pathologists alike due to its complex diagnostic landscape and therapeutic implications. A recent comprehensive study conducted at a leading tertiary care cancer referral center in India delves into the clinico-pathological, immunohistochemical, and molecular profiles of synovial sarcoma, revealing critical insights that may refine diagnosis and treatment strategies for this rare yet impactful disease.
The hallmark of synovial sarcoma lies within its genetic signature: the pathognomonic chromosomal translocation t(X;18)(p11;q11). This aberration results in the fusion of the SS18 gene to one of the SSX family genes, predominantly SSX1 or SSX2, generating the SS18:SSX fusion oncogenes. These fusion proteins drive oncogenesis through mechanisms that disturb epigenetic regulation and promote oncogenic transcriptional programs. Understanding these molecular underpinnings is vital for establishing precise diagnostic criteria and targeting therapeutic interventions.
This retrospective observational study, spanning four years, encompassed 108 patients fulfilling rigorous inclusion and exclusion criteria, providing a robust dataset to investigate the heterogeneity of synovial sarcoma. The median age of the cohort was 30.5 years, underscoring the tumor’s predilection for younger individuals. The mean tumor size was considerable at 10.5 cm, reflecting a pattern of late presentation or rapid tumor growth that poses challenges for effective management.
Anatomically, the lower limb emerged as the predominantly affected site, followed sequentially by the lung and upper limb regions such as the arm. This distribution points to the versatile nature of synovial sarcoma, which can originate in diverse soft tissue compartments. Such anatomical variability necessitates a high index of suspicion and comprehensive pathological evaluation to avoid misdiagnosis, particularly in non-extremity locations.
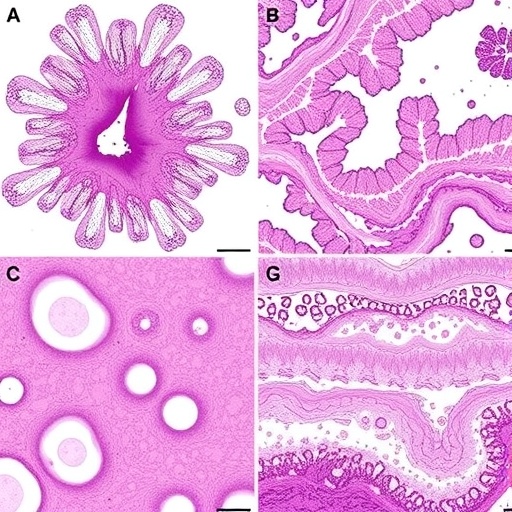
Morphological categorization revealed that 81% of cases exhibited the monophasic subtype, characterized primarily by spindle cells, while 19% demonstrated the biphasic subtype, which includes both spindle and epithelial components. This distinction, while classical, is not always straightforward. The overlap in histology with other spindle cell neoplasms necessitates adjunct diagnostic modalities beyond morphology alone.
Immunohistochemistry (IHC) remains indispensable for clarifying diagnostic ambiguity. This study identified key markers that significantly aid in the confirmation of synovial sarcoma. TLE1, a transcriptional corepressor, showed strong diagnostic utility, in combination with epithelial membrane antigen (EMA), pancytokeratin, S-100 protein, BCL2, and CD99. The panel approach facilitates differentiation from morphologically similar entities such as malignant peripheral nerve sheath tumors and solitary fibrous tumors, which may share some overlapping IHC staining patterns.
A subset of 15 patients underwent molecular diagnostic evaluation to confirm the presence of the SS18 gene rearrangement, the definitive hallmark for verifying synovial sarcoma. Molecular techniques such as fluorescence in situ hybridization (FISH) or reverse transcription polymerase chain reaction (RT-PCR) confirmed this genetic translocation in two-thirds of tested patients, highlighting both the strengths and limitations of molecular diagnostics in routine clinical practice.
Clinically, the management of synovial sarcoma primarily hinges on complete surgical excision with negative margins to minimize local recurrence. In the cohort analyzed, 50 patients underwent surgical resection, complemented by adjuvant therapies—chemotherapy or radiotherapy—in 49 patients. The therapeutic regimens were tailored based on individual patient and tumor characteristics, underscoring a multidisciplinary approach that optimizes outcomes in this aggressive disease.
The follow-up interval in this study averaged 7.58 months, with survival analysis indicating a promising 4-year overall survival rate of 91.39%. This favorable outcome potentially reflects advances in surgical techniques, adjuvant therapies, and early diagnostic accuracy. Nevertheless, the relatively short follow-up demands cautious interpretation, advocating for longer-term studies to substantiate these encouraging results.
The study’s findings emphasize the imperative role of pathologists’ expertise in recognizing both typical and variant histologies of synovial sarcoma. Integrating morphology with immunohistochemical profiling and molecular confirmation fosters diagnostic precision, especially in cases with atypical presentations. Such comprehensive evaluation is invaluable in tertiary referral centers where diagnostic complexity demands sophisticated approaches.
Beyond diagnostic challenges, the molecular biology of synovial sarcoma offers fertile ground for therapeutic innovation. The SS18:SSX fusion protein modulates chromatin remodeling complexes and disrupts cellular differentiation pathways, making it an attractive target for precision medicine. Efforts are underway to develop small molecules and immunotherapeutic strategies aimed at thwarting the oncogenic consequences of this fusion, promising to transform the therapeutic landscape.
This investigation from India enriches global understanding by illuminating epidemiological and pathological nuances in a demographically distinct population. The large patient cohort offers statistical power to discern patterns that may differ in geographic and ethnic contexts, highlighting the need for region-specific data to inform clinical guidelines and public health strategies.
The meticulous design and execution of this study showcase the integration of clinicopathological data with modern molecular insights, establishing a benchmark for future research endeavors. The interdisciplinary collaboration between oncologists, pathologists, and molecular biologists exemplifies the holistic approach necessary to combat complex sarcomas effectively.
Ultimately, managing synovial sarcoma demands balancing aggressive local control through surgery with systemic therapies guided by tumor biology. Continued research into immunohistochemical markers beyond the classical panel may further refine diagnostic accuracy, and emerging genomic technologies promise to unveil additional molecular aberrations with prognostic and therapeutic relevance.
As synovial sarcoma remains a formidable adversary in the oncology realm, advances in diagnostic precision, molecular characterization, and tailored therapies herald a new era of hope. The insights revealed by this Indian tertiary center study underscore the critical importance of combining traditional pathology with cutting-edge molecular diagnostics to improve patient outcomes worldwide.
Subject of Research: Clinicopathological, immunohistochemical, and molecular features of synovial sarcoma across organ systems.
Article Title: Evaluating the clinico-pathological features including the immunohistochemical and molecular landscape of synovial sarcoma cases from a tertiary care cancer referral centre in India.
Article References:
Rai, H., Dhal, I., Chowdhury, Z. et al. Evaluating the clinico-pathological features including the immunohistochemical and molecular landscape of synovial sarcoma cases from a tertiary care cancer referral centre in India. BMC Cancer 25, 1445 (2025). https://doi.org/10.1186/s12885-025-14862-x
Image Credits: Scienmag.com