In a groundbreaking study, researchers have unveiled a compelling connection between hypoxia—the condition where there is a deficiency of oxygen—and the functioning of microglial cells in relation to beta-amyloid peptides, which are pivotal in the development of neurodegenerative diseases like Alzheimer’s. This research, published in the Journal of Translational Medicine, provides intriguing insights into how the brain’s immune system may inadvertently contribute to neurodegeneration in low-oxygen environments, a condition that can commonly occur in various pathological states, including chronic neurodegenerative diseases.
Microglial cells, the brain’s resident immune cells, are critical players in maintaining homeostasis within the central nervous system. They are known for their ability to respond to injury and disease by adopting an anti-inflammatory role early on, which is essential for the repair and recovery process. However, in conditions of hypoxia, this beneficial response appears to be altered dramatically. The study’s authors, led by Lipari, highlight how microglial cells, when exposed to low oxygen environments, reverse their protective anti-inflammatory activities. This reversal could potentially accelerate the accumulation of beta-amyloid peptides, exacerbating neurodegenerative processes and cognitive decline.
At the core of this research lies the examination of mitochondrial function in microglial cells. Mitochondria, often referred to as the powerhouses of the cell, play a crucial role in energy production and maintaining cellular health. In instances of hypoxia, mitochondrial efficiency significantly declines, leading to an energy crisis within cells. This study provides evidence that such a crisis is not only detrimental to neuronal health but also alters the functional state of microglial cells, leading to a shift away from their typically protective roles. The authors suggest that these cellular metabolic dysfunctions are a key factor in the interplay between hypoxia and microglial response to beta-amyloid.
In addition to identifying the detrimental effects of hypoxia on microglia, the researchers also explored potential therapeutic interventions. They investigated the roles of melatonin and naringenin—two compounds known for their antioxidant and anti-inflammatory properties. Melatonin, a hormone that regulates sleep and circadian rhythms, has been previously identified for its neuroprotective abilities. Naringenin, a flavonoid commonly found in citrus fruits, exhibits a variety of biological activities, including anti-inflammatory and neuroprotective effects.
The findings from this study indicate that both melatonin and naringenin could play protective roles in countering the adverse effects of hypoxia on microglial function. The administration of these compounds to cultured microglia under hypoxic conditions restored some of their anti-inflammatory properties. This raises the possibility of developing new therapeutic strategies to enhance the resilience of microglial cells in the face of hypoxic stress, potentially mitigating neurodegenerative processes associated with Alzheimer’s disease.
The research presents a significant shift in our understanding of how microglial cells respond to environmental stressors. It suggests that rather than being universally protective, microglia can flip their functional states under the duress of insufficient oxygen. This change can lead to a diminished capacity to clear harmful proteins such as beta-amyloid, which are known to form plaques in the brains of Alzheimer’s patients, thereby contributing to cognitive decline.
Moreover, the implications of this study extend beyond Alzheimer’s disease. Understanding how low oxygen levels influence immune responses in the brain could provide crucial insights into various other neurological disorders. Conditions like multiple sclerosis, stroke, and traumatic brain injuries often involve hypoxia, indicating that the findings may have broader relevance in the field of neurobiology and immunology.
While this study uncovers critical connections between hypoxia, microglial function, and neurodegeneration, it also opens new avenues for research. Future studies could focus on delineating the exact mechanisms by which hypoxia alters microglial metabolism and function. They may also explore the potential of melatonin and naringenin not just as treatments but also as preventive measures for at-risk populations.
Further investigations could involve clinical trials to assess the therapeutic efficacy of these compounds in humans, particularly in populations with early indications of Alzheimer’s or other neurodegenerative diseases. There is also potential to explore additional agents that may support microglial health in hypoxic conditions, broadening the potential for novel treatment protocols.
This study is a reminder of the intricate relationships between cellular environments and immune responses, particularly in the brain. The findings underscore the importance of restoring homeostasis in the central nervous system as a pathway toward preventing or mitigating the impacts of diseases characterized by neurodegeneration.
Broader research implications may lead to a shift in how neurologists approach treatment strategies for Alzheimer’s and other similar conditions. Understanding the dual roles that microglial cells may play—not only as protectors but also as potential perpetrators of neurodegeneration—could reframe therapeutic goals.
As research advances, the evolution of targeted therapies could significantly enhance the quality of life for patients suffering from Alzheimer’s and related disorders. Harnessing the potential of natural compounds like melatonin and naringenin may not only prove beneficial in clinical settings but also pave the way for innovative biopharmaceutical approaches aimed at restoring balance within the brain’s immune system, ultimately aiming for better outcomes for individuals battling these debilitating diseases.
In conclusion, the study by Lipari and colleagues provides valuable insights into the complex dynamics of hypoxia, microglial response, and neurodegeneration, emphasizing the urgent need for continued exploration in this crucial area of neuroscience.
Subject of Research: The effect of hypoxia on microglial response to β-amyloid peptides and the potential therapeutic roles of melatonin and naringenin.
Article Title: Hypoxia reverses the early anti-inflammatory microglial response to the β-amyloid peptide: mitochondrial involvement and beneficial roles of melatonin and naringenin.
Article References:
Lipari, C.L.R., Patti, A., Conti-Nibali, S. et al. Hypoxia reverses the early anti-inflammatory microglial response to the β-amyloid peptide: mitochondrial involvement and beneficial roles of melatonin and naringenin.
J Transl Med 23, 1012 (2025). https://doi.org/10.1186/s12967-025-07044-7
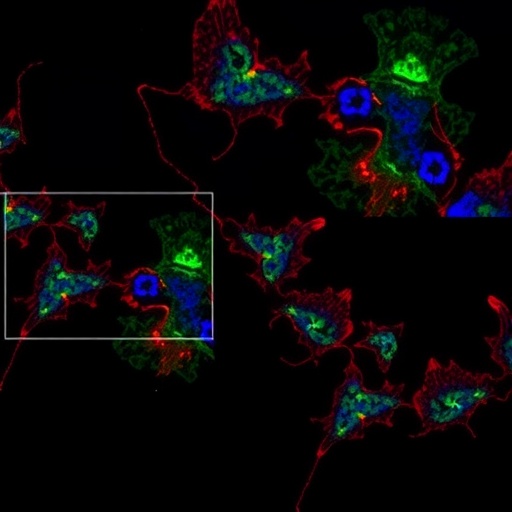
Image Credits: AI Generated
DOI: 10.1186/s12967-025-07044-7
Keywords: hypoxia, microglia, beta-amyloid, melatonin, naringenin, neurodegeneration, Alzheimer’s disease, mitochondrial function, anti-inflammatory response.