In a landmark advance that could reshape the landscape of organ transplantation, researchers have reported the unprecedented successful implantation of a genetically engineered pig kidney into a living human, maintaining stable physiologic homeostasis over an extended period. This breakthrough study, published in Nature Communications, demonstrates the potential of xenotransplantation to alleviate the critical shortage of human donor organs and paves the way for revolutionary new therapies for patients with end-stage renal disease.
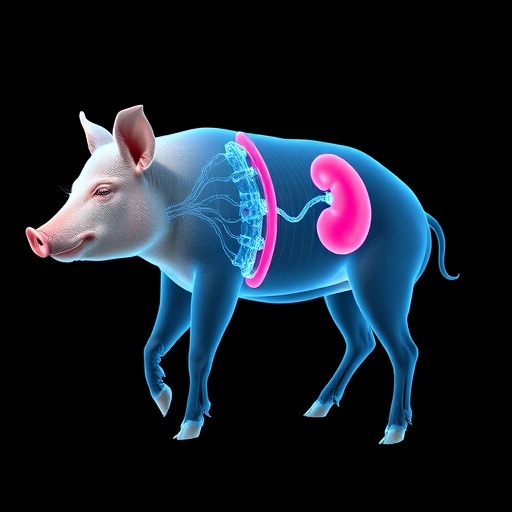
The intricate biological barriers that have long impeded cross-species organ transplantation—immunologic rejection, blood incompatibilities, and zoonotic infections—have historically rendered such procedures nonviable. However, with cutting-edge gene-editing technologies, the scientific team engineered the donor pig kidney to address these challenges. By silencing pig antigens responsible for acute rejection and introducing human genes to improve compatibility, the researchers created a biosimilar organ capable of circumventing hyperacute immune responses in the human recipient.
The subject who received the xenotransplant was a carefully selected adult patient suffering from irreversible renal failure who was ineligible for conventional human kidney transplantation due to sensitization or other comorbidities. Under rigorous clinical supervision, an ex vivo normothermic perfusion technique was employed to preserve the pig kidney post-harvest and optimize its function before implantation. This method maintains oxygen and nutrient delivery, mitigating ischemic injury and encouraging immediate graft viability once transplanted.
Upon implantation, the pig kidney integrated seamlessly with the recipient’s circulatory system, with continuous monitoring revealing normalized urine production, stable electrolyte balance, and controlled blood pressure regulation. Notably, comprehensive immunosuppressive protocols were administered, aiming to finely balance immune tolerance without predisposing the patient to infection or malignancy. Vital parameters remained stable throughout, with no evidence of hyperacute or antibody-mediated rejection episodes, an extraordinary outcome given previous preclinical models.
The research team further conducted in-depth metabolic and immunologic profiling, confirming that the xenograft maintained efficient glomerular filtration rates comparable to those of a healthy human kidney. Biomarkers associated with renal tubular function and acid-base homeostasis remained within physiologic parameters, underscoring the organ’s functional integrity. Additionally, no cross-species infectious transmissions were detected through extensive screening, alleviating concerns about porcine endogenous retroviruses (PERVs) and other zoonoses.
Central to the success of this intervention was the sophisticated gene editing of the donor pig to eliminate about 10 susceptibility genes that encode carbohydrate antigens such as alpha-gal and Neu5Gc, key targets for the human natural antibody repertoire. Furthermore, human complement regulatory proteins and thromboregulatory genes were inserted to modulate inflammatory cascades and prevent microvascular thrombosis, a frequent complication in xenotransplanted organs. This unprecedented level of genomic tailoring represents a milestone in synthetic biology applications in medicine.
This trial marks the first time a pig kidney has functioned physiologically in a living human long enough to demonstrate sustained homeostasis, contributing valuable insights into the organ’s systemic effects beyond filtration. The investigators tracked hemodynamic indices, hormonal responses including renin-angiotensin system activity, and electrolyte handling, which collectively supported the conclusion that the xenograft was not only functional but actively integrated within the recipient’s homeostatic mechanisms.
Beyond renal replacement, the implications of this success extend to other organ systems where transplantation demand far exceeds supply. Heart, liver, and lung xenotransplantations remain experimental, but this groundbreaking kidney transplant provides a proof-of-concept validating the feasibility of long-term xenografts under carefully optimized immunological and genetic conditions. Future studies will investigate multi-organ compatibility and refined immunomodulation strategies.
The ethical and regulatory dimensions of introducing animal organs into humans were rigorously addressed by the research consortium. Institutional review boards and regulatory agencies mandated comprehensive informed consent, transparent risk-benefit assessment, and meticulous biosafety protocols. Societal perception and cultural considerations around xenotransplantation will require ongoing dialogue, based on empirical evidence generated from pioneering trials like this one.
From a technological viewpoint, advances in CRISPR-Cas9 gene-editing facilitated the precision required to edit multiple loci in the porcine genome simultaneously. The scalability and repeatability of these modifications herald vast potential for customized xenogeneic organ sources. Additionally, the research incorporated next-generation biomaterials and bioinformatics tools to monitor graft viability non-invasively, signaling a new paradigm in transplant medicine.
The documented absence of rejection and the establishment of stable renal physiological control over weeks post-transplant serves as a critical benchmark for future clinical translation. The authors emphasize that while this milestone is monumental, xenotransplantation will necessitate further refinement in immunosuppressive regimens and long-term safety evaluations before widespread adoption. Nonetheless, this achievement rekindles hope for the millions waiting for lifesaving organ transplants worldwide.
This study also reignites debate on the role of biotechnology in addressing organ scarcity, highlighting the convergence of genetics, immunology, and regenerative medicine. The capacity to engineer organs from animal sources, circumvent human donor limitations, could revolutionize healthcare economics, reducing waitlist mortality and enhancing quality of life for patients with terminal organ dysfunction.
Moreover, the physiological data collected provide unprecedented insights into interspecies organ compatibility at an unparalleled resolution, informing both clinical and basic science domains. The research delineates pathways of cross-species immunologic tolerance potentially fundamental to one day generating fully humanized organs from xenogeneic tissues through advanced chimeric or stem cell technologies.
In conclusion, this remarkable demonstration of physiologic homeostasis in a living human following pig kidney xenotransplantation represents a turning point in transplantation science. By overcoming formidable immunological and biological barriers, the authors have managed to sustain vital kidney functions with a xenograft, underscoring the promise of genetically engineered animal organs in expanding the transplant donor pool and transforming patient outcomes globally.
As the global medical community eagerly anticipates subsequent trials building upon this foundation, the potential ramifications resonate well beyond nephrology. This pioneering success signals a dawn of synthetic and transplant medicine synergy, illuminating a future where organ shortages may become a relic of the past and innovative therapies redefine the boundaries of human health and longevity.
Subject of Research:
Physiologic homeostasis and functional integration of a genetically engineered pig kidney xenotransplanted into a living human recipient.
Article Title:
Physiologic Homeostasis in a Living Human after Pig Kidney Xenotransplantation.
Article References:
Lee, S.A., Lafargue, M.C., Williams, W.W. et al. Physiologic Homeostasis in a Living Human after Pig Kidney Xenotransplantation. Nat Commun 16, 8453 (2025). https://doi.org/10.1038/s41467-025-63153-3
Image Credits: AI Generated