In a groundbreaking study published in Nature Cell Biology, scientists from St. Jude Children’s Research Hospital have unveiled a pivotal role for lipids in the initiation of LC3-associated phagocytosis (LAP), a specialized cellular degradation process integral to immune system function and cancer biology. This discovery opens new horizons for therapeutic modulation of immune responses in cancer and beyond, by elucidating how membrane lipids orchestrate the molecular events that trigger LAP.
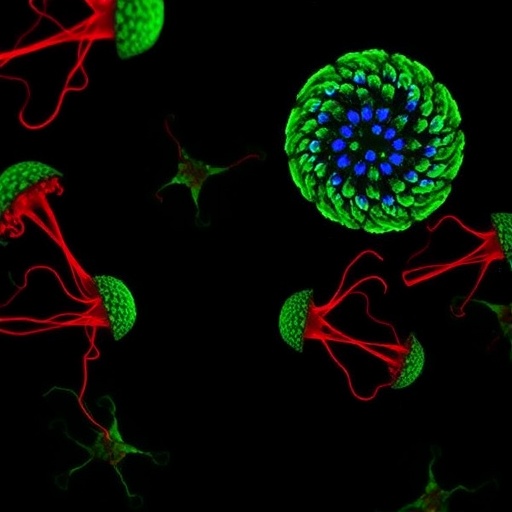
LC3-associated phagocytosis is a sophisticated cellular mechanism by which specialized immune cells engulf and degrade unwanted materials, including dead cells, pathogens, and antibody-coated particles. Through this process, phagocytic cells internalize external cargo into membrane-bound vesicles known as phagosomes. Subsequently, the autophagy-related protein LC3 is conjugated to the phagosomal membrane, facilitating the breakdown and recycling of the engulfed material. This distinct pathway serves not only in maintaining tissue homeostasis but also in regulating inflammation and modulating anticancer immune responses within the tumor microenvironment.
While the significance of LAP in immune regulation and cancer progression has been increasingly appreciated, the molecular signals that initiate this pathway have remained elusive until now. The diversity of stimuli capable of triggering LAP prompted a fundamental question: how do cells integrate disparate recognition signals to activate a conserved intracellular machinery? Addressing this knowledge gap, the research team led by Dr. Doug Green and first author Dr. Emilio Boada-Romero employed advanced experimental approaches to dissect the signaling cascade that prompts LAP initiation.
Their investigation revealed that phosphatidylserine (PS), a negatively charged lipid conventionally localized to the inner leaflet of cellular membranes, plays a central role in this process. Upon ligand engagement during phagocytosis, PS becomes enriched on the cytosolic face of the phagosomal membrane. This lipid enrichment functions as a biochemical beacon, recruiting the Rubicon-containing phosphatidylinositol 3-kinase (PI3K) complex necessary for activating downstream enzymatic effectors that attach LC3 to the membrane, thereby initiating LAP.
This paradigm-shifting insight highlights a nuanced form of lipid signaling wherein phosphatidylserine acts beyond its structural role, serving as a critical regulatory platform for protein complex assembly. The finding that PS clustering at phagosomal membranes orchestrates the intracellular activation of LAP bridges a significant gap in understanding the interface between membrane biophysics and immune cell signaling.
Importantly, by identifying phosphatidylserine as a functional docking site in LAP, this work links membrane lipid dynamics to the modulation of immune responses. Previous studies had shown that impairment of LAP enhances anticancer immunity by altering macrophage behavior in tumor environments. The current discovery suggests that manipulating PS exposure or its downstream signaling interactions may provide innovative strategies to reprogram macrophage activity and potentiate antitumor immunity.
The study also underscores the multifaceted roles of membrane lipids in immune regulation. Phagocytosis inherently involves complex membrane remodeling events, and these findings emphasize that specific lipid species are active participants, not mere structural components, in determining the fate of phagosomal cargo and the immunological outcomes of engulfment. Such insights extend to broader contexts including autoimmunity, infection, and tissue repair, where LAP similarly influences disease progression.
Moreover, elucidating a lipid-driven initiation mechanism reconciles the observation that LAP can be triggered by an array of stimuli, each promoting PS clustering, thus providing a unified molecular explanation for LAP activation. This lipid-centric model deepens our mechanistic understanding and may guide the development of lipophilic or lipid-targeting molecules aimed at fine-tuning LAP activity.
This pioneering research was carried out by a collaborative team at St. Jude, including Clifford Guy, Gustavo Palacios, Luigi Mari, Suresh Poudel, Zhenrui Li, and Piyush Sharma, under the leadership of Dr. Green and Dr. Boada-Romero. Their study was generously supported by funding from the U.S. National Institutes of Health, the European Molecular Biology Organization, and ALSAC, enabling comprehensive experimental investigation into the crosstalk between lipid signaling and innate immunity.
Beyond its fundamental scientific impact, the identification of phosphatidylserine’s role in LAP initiation offers promising translational potential. Therapeutic approaches that modulate lipid distribution or target the Rubicon-containing PI3K complex might be harnessed to either amplify or inhibit LAP, tailoring immune responses to treat cancer, chronic inflammation, and autoimmune diseases more effectively. This adds a novel lipid dimension to immunotherapy that complements existing antibody- and cell-based treatments.
Dr. Doug Green remarked on the translational significance of these findings, stating that understanding the signals activating LAP could empower researchers to “leverage LAP for therapeutic purposes,” particularly in reshaping the immune landscape within tumors. Dr. Emilio Boada-Romero noted that uncovering phosphatidylserine’s role “adds an exciting layer” to lipid biology and immune regulation, highlighting the intricate interplay between membrane composition and cellular function.
As the first evidence connecting specific lipids to the regulation of LAP, this research sets the stage for further exploration into lipid-mediated signal transduction pathways in immunity. It advances a frontier in cellular immunology where bioactive lipids are recognized as crucial modulators of immune cell behavior, with implications extending to pathogen defense mechanisms and immunometabolic disorders.
In conclusion, the discovery of a phosphatidylserine-driven mechanism initiating LC3-associated phagocytosis marks a transformative advancement in our grasp of immune cell biology. By linking membrane lipid dynamics to essential degradation pathways and immune modulation, this study not only fills a vital mechanistic gap but also provides a fertile ground for innovative therapeutic strategies aimed at harnessing the immune system in disease intervention.
Subject of Research: Cells
Article Title: Membrane receptors cluster phosphatidylserine to activate LC3-associated phagocytosis
News Publication Date: 22-Sep-2025
Image Credits: Courtesy of St. Jude Children’s Research Hospital
Keywords: Cancer