In a groundbreaking discovery that sheds new light on the metabolic underpinnings of atherosclerosis, researchers have illuminated the pivotal role of the amino acid glutamine in controlling macrophage behavior within arterial plaques. The study, led by Benhmammouch et al. and published in Nature Metabolism in 2025, elucidates how the critical membrane transporter SLC7A7 orchestrates glutamine uptake and subsequent glutaminolysis, thereby shaping macrophage restorative functions essential for plaque stability. This insight may catalyze a paradigm shift in targeting macrophage metabolism to combat atherosclerotic disease, a leading cause of cardiovascular morbidity and mortality worldwide.
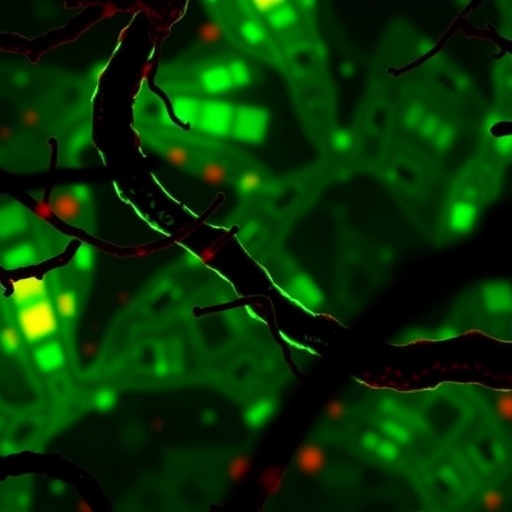
Atherosclerosis, a chronic inflammatory disease of the arterial wall, is chiefly driven by the accumulation of lipids and immune cells, prominently macrophages, within the vessel intima. These macrophages exhibit remarkable plasticity, adapting their metabolic and functional phenotype to the local microenvironment. While previous studies have implicated metabolic rewiring in macrophage-driven inflammation, the specific molecular mechanisms linking nutrient flux to macrophage behavior in plaques remained elusive. This new study clarifies this mechanism by focusing on glutamine metabolism, a key metabolic pathway that governs cellular bioenergetics and redox homeostasis.
The team’s investigation revealed that glutaminase 1 (GLS1), rather than its isoform GLS2, dominantly orchestrates glutaminolysis in macrophages located within atherosclerotic plaques. Glutaminase catalyzes the conversion of glutamine into glutamate, feeding into the tricarboxylic acid (TCA) cycle to support energy production and biosynthesis. Intriguingly, while glutamine synthetase can regulate the synthesis of glutamine and function as a rheostat controlling nutrient flux in vitro, the macrophage use of glutamine within plaques was less reliant on endogenous generation and profoundly dependent on external glutamine uptake.
Central to this glutamine uptake is the cationic amino acid transporter SLC7A7, which facilitates the influx of glutamine into macrophages. Silencing experiments demonstrated that disruption of Slc7a7 expression sharply reduced glutamine influx as well as GLS1-mediated glutaminolysis. This blockade in metabolic flux impaired key downstream signaling pathways that underlie macrophage restorative, as opposed to inflammatory, functions. These findings highlight SLC7A7 as a crucial metabolic gatekeeper, ensuring that macrophages within plaques access sufficient glutamine to execute reparative programs.
By employing macrophage-specific Slc7a7 knockout mouse models of atherosclerosis, the researchers illuminated the in vivo relevance of their findings. Mice deficient in macrophage Slc7a7 exhibited accelerated plaque progression marked by an increase in necrotic core complexity, an indicator of lesion instability and heightened risk of plaque rupture. The study eloquently connects impaired glutamine uptake with impaired macrophage function and worsened disease phenotype, directly linking amino acid metabolism to clinical outcomes in cardiovascular pathology.
At the cellular level, the absence of Slc7a7 frustrated the ability of macrophages to balance functional remodeling and restorative activities, processes essential for plaque maintenance and regression. Macrophages deprived of glutamine exhibited altered metabolic and transcriptional landscapes, underscoring the profound influence of nutrient availability on immune cell programming. This cell-intrinsic metabolic shift orchestrated by glutaminolysis plays a determinant role in macrophage fate and function within the diseased vasculature.
The implications of this research are manifold. It challenges prior assumptions that macrophage metabolic states are predominantly fixed and inflexible in chronic inflammation and underscores the potential of targeting amino acid transporters to fine-tune immune responses. By elevating SLC7A7 to a position of therapeutic interest, this study opens avenues for the development of metabolic interventions that recalibrate macrophage function, potentially stabilizing plaques and preventing adverse cardiovascular events.
Moreover, the innovative use of a metabolic rheostat concept, wherein glutamine synthetase adjusts intracellular glutamine levels dynamically, adds nuance to our understanding of nutrient flux regulation. The finding that glutamine influx via SLC7A7 outranks glutamine synthesis capacity in macrophage functional specialization within plaques is a novel insight, emphasizing the importance of extracellular nutrient sourcing in shaping immune cell metabolism.
The interplay between glutamine metabolism and macrophage phenotypic plasticity emerges as a critical factor in vascular health, reinforcing the notion that immunometabolism is integral to disease progression. Future therapeutic strategies could harness this axis, employing small molecules or biologics to modulate SLC7A7 activity or glutaminolysis pathways, providing a precision medicine approach to combat cardiovascular disease.
Technically, the study employed a combination of transcriptomic profiling, metabolic flux analyses, and sophisticated in vivo genetic manipulations to unravel the intricate connections between Slc7a7, glutaminolysis, and macrophage function. This multi-dimensional approach firmly establishes a causal relationship and highlights the utility of integrated methods in understanding complex metabolic networks within pathological contexts.
While glutamine has long been recognized as a versatile metabolite involved in cellular growth and immune regulation, this research uniquely positions glutamine uptake as a rate-limiting step modulated by SLC7A7 in the context of chronic arterial inflammation. The specificity of this transporter’s role challenges the field to reevaluate how amino acid transporters contribute to metabolite partitioning and immune cell fate decisions in situ.
Furthermore, the accelerated plaque progression observed in Slc7a7-deficient macrophages may have broader implications beyond atherosclerosis, potentially informing our understanding of other chronic inflammatory diseases where macrophage-mediated repair is compromised. The metabolic tuning of immune cells by extracellular amino acid availability could be a universal mechanism in tissue homeostasis and pathology.
This comprehensive analysis of macrophage glutamine metabolism in atherosclerosis not only charts new territory but also bridges metabolism with immunology and vascular biology, enriching our toolkit to confront one of the leading causes of death worldwide. As researchers continue to dissect the metabolic determinants of immune cell function, the role of transporters like SLC7A7 is poised to emerge prominently in the design of future therapeutic interventions.
In conclusion, the identification of SLC7A7 as a critical facilitator of macrophage glutaminolysis and restorative function within atherosclerotic plaques underscores the complexity and potential of targeting cellular metabolism to modulate disease. This work exemplifies how a deep mechanistic understanding of immune cell metabolism can translate into clinically relevant insights with transformative potential for cardiovascular medicine.
Subject of Research: Macrophage glutamine metabolism and its role in atherosclerosis progression and plaque stability.
Article Title: Slc7a7 licenses macrophage glutaminolysis for restorative functions in atherosclerosis.
Article References:
Benhmammouch, S., Borowczyk, C., Pierrot-Blanchet, C. et al. Slc7a7 licenses macrophage glutaminolysis for restorative functions in atherosclerosis. Nat Metab (2025). https://doi.org/10.1038/s42255-025-01354-2
Image Credits: AI Generated