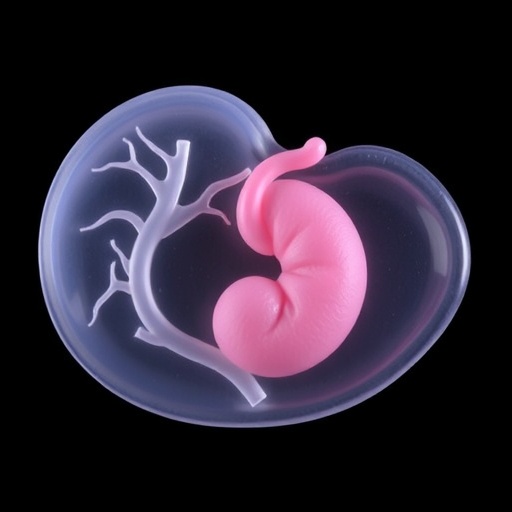
In a groundbreaking advancement that promises to revolutionize our understanding of pregnancy complications, scientists at the University of Technology Sydney (UTS) have successfully 3D bioprinted miniature placentas, or placenta organoids, offering an unprecedented window into early placental development. This achievement holds immense potential for unraveling the complex biological mysteries that underpin conditions like preeclampsia, a serious pregnancy disorder linked to placental dysfunction and affecting millions globally. By harnessing cutting-edge bioprinting technology, the research team has set the stage for transformative breakthroughs in prenatal medicine, drug testing, and ultimately, maternal and infant health.
The placenta is a remarkable yet enigmatic organ, critical for sustaining pregnancy by facilitating nutrient and oxygen exchange between mother and fetus. However, studying the placenta in early pregnancy remains extraordinarily difficult. Ethical and practical constraints limit access to first-trimester placental tissue, while samples obtained at birth no longer accurately represent the placenta’s initial state due to extensive changes during gestation. This challenge has long stifled deeper insight into pregnancy pathologies such as preeclampsia, a condition characterized by high blood pressure and organ damage in the mother, contributing to over 260,000 maternal deaths annually worldwide.
To bridge this knowledge gap, the team led by Associate Professor Lana McClements and Dr Claire Richards from the UTS School of Life Sciences focused on creating a biomimetic model of the early human placenta using 3D bioprinting. Unlike conventional manual methods where cells grow within animal-derived gels, their approach intricately combines trophoblast cells—specialized cells exclusive to the placenta—with a synthetic, tunable hydrogel, then precisely deposits this bioink using an inkjet-style bioprinter. Such a technique allows the researchers to control the structural and biochemical environment surrounding the cells, steering their organization and differentiation in ways not previously achievable.
Organoids, miniature organ-like structures derived from stem cells or progenitors, have revolutionized biomedical research since their inception in 2009. These miniaturized models recapitulate key aspects of organ structure and function in vitro, serving as powerful platforms to investigate tissue development, disease mechanisms, and drug responses. In 2018, the first placental organoids were cultivated from trophoblast cells isolated from term placentas. However, these organoids lacked the spatial precision and microenvironment control necessary to faithfully model the earliest stages of placental growth, especially during the critical period of embryo implantation and vascularization.
Bioprinting technologies bring a new dimension to organoid generation. By depositing living cells in three-dimensional patterns with spatial precision, bioprinting can recreate the intricate architectures and cellular microenvironments found in vivo. In this study, the researchers employed a synthetic matrix capable of fine-tuning mechanical stiffness and biochemical signals, which strongly influence trophoblast differentiation pathways. This synthetic approach sidesteps the batch variability and animal-origin concerns associated with traditional extracellular matrices, enabling standardized and reproducible placental models ideal for experimental rigor.
Comparative analyses between bioprinted organoids and those generated manually revealed distinct differences in trophoblast subtype composition and maturation trajectories, suggesting that the cellular milieu and physical context significantly modulate placental development. These findings underscore the critical importance of the extracellular matrix in dictating cell fate decisions during early gestation. Importantly, the bioprinted organoids exhibited remarkable similarity to in vivo human placental tissue at the molecular and functional levels, validating their relevance as accurate models of early placenta.
Harnessing this novel platform, the researchers simulated pathogenic conditions by exposing bioprinted organoids to inflammatory molecules elevated in women with preeclampsia. The organoids’ responses to these stimuli, including altered growth and differentiation patterns, were then monitored, providing key insights into disease mechanisms. Moreover, the team tested candidate therapeutics on these inflamed organoids, demonstrating the model’s utility for preclinical drug screening and safety evaluation, a significant step toward personalized treatment strategies for pregnancy complications.
The implications of this research extend far beyond the laboratory. With pregnancy complications such as preeclampsia remaining a leading cause of maternal and infant morbidity and mortality worldwide, robust in vitro models that faithfully mimic early placental biology are urgently needed. Bioprinted placenta organoids could fuel drug discovery pipelines, reduce reliance on animal models, and accelerate the development of interventions that prevent or mitigate adverse pregnancy outcomes.
The study also exemplifies the broader promise of bioprinting in regenerative medicine and developmental biology. By enabling the construction of human tissue models with precise control over cellular composition and mechanical environment, bioprinting paves the way for personalized medicine applications, disease modeling, and potentially even the fabrication of transplantable tissues in the future.
As research progresses, refining these organoid models will be crucial. This includes integrating additional placental cell types such as endothelial and immune cells, constructing vascularized structures, and incorporating maternal-fetal interface components to fully capture the complexity of the placental microenvironment. Such advancements will undoubtedly deepen our understanding of placental physiology and pathology, ensuring safer pregnancies and healthier newborns.
In conclusion, the pioneering work by UTS researchers marks a significant milestone in reproductive science. Through the innovative application of 3D bioprinting, they have created a sophisticated model of the early human placenta that promises to unlock the secrets of pregnancy complications. As these models evolve, they hold the potential to revolutionize prenatal healthcare by enabling early detection, prevention, and treatment of disorders that currently threaten the lives of mothers and infants worldwide.
Subject of Research: Cells
Article Title: Matrix directs trophoblast differentiation in a bioprinted organoid model of early placental development
News Publication Date: Not specified (Article published 12-Sep-2025)
Web References:
DOI: 10.1038/s41467-025-62996-0
Article in Nature Communications
Image Credits: Images acquired at the UTS Microbial Imaging Facility by Dr Claire Richards
Keywords: 3D bioprinting, placenta organoids, trophoblast differentiation, preeclampsia, pregnancy complications, synthetic matrix, early placental development, regenerative medicine, prenatal drug testing, maternal-fetal health