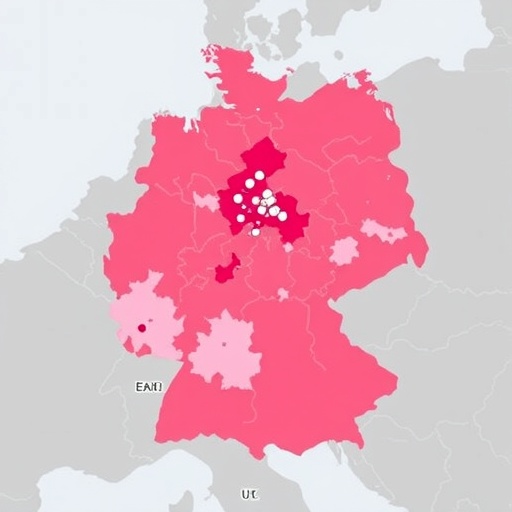
In a groundbreaking initiative driven by the ONCOnnect consortium, researchers have embarked on an ambitious project to better understand the catchment areas of comprehensive cancer centers across Germany. Leveraging geographic healthcare data, the study provides critical insights into how these centers serve patients and the geographic disparities that may persist in cancer care access. The findings are not just statistical; they weave a narrative of accessibility and patient care that has profound implications for cancer treatment and healthcare planning in the nation.
The researchers focused on the intricate web of healthcare systems in Germany, where comprehensive cancer centers are strategically located to provide essential services. However, the effectiveness of these centers in reaching their intended populations hinges on understanding the geographic factors that define their catchment areas. By merging various health data sources, the researchers aimed to create a clearer picture of how distance and demographics impact patient access to vital oncology services.
Geographic disparities in healthcare access are a well-documented issue, particularly in cancer care. Patients often face significant barriers such as travel distance, socioeconomic factors, and regional health policies that can influence their ability to receive timely and effective treatment. The ONCOnnect consortium’s study highlights these challenges, emphasizing the need for a focused approach to bridge the gap between healthcare availability and patient needs. As part of the analysis, researchers used advanced geographic information systems (GIS) to analyze data sets that include population density, transportation networks, and existing healthcare facilities.
One of the pivotal aspects of this study is its emphasis on data integrity and cross-referencing various sources. Geographic healthcare data was merged from multiple databases to form a comprehensive view of cancer care distribution across the nation. The researchers meticulously ensured that the data was up-to-date and relevant, noting any discrepancies that could arise from outdated or uncoordinated records. This meticulous attention to detail is crucial, as accurate data forms the bedrock of effective healthcare planning.
Cancer patients often experience delays in seeking care, a phenomenon that can be exacerbated by the geography of healthcare providers. Recognizing this, the research aimed to spotlight regions where access to cancer centers is limited, highlighting the possibility of developing targeted interventions. These interventions could be in the form of mobile care units, telemedicine services, or community outreach programs designed to bring awareness and resources to underserved areas.
The findings of the study are expected to influence not only policy within the healthcare system but also funding allocations for cancer care within Germany. By identifying which areas are most at risk of being underserved, policymakers can make informed decisions about where to invest their resources. Additionally, the implications extend beyond immediate healthcare planning; they may also encourage collaboration among various stakeholders, including local governments, healthcare providers, and cancer advocacy groups, to address the disparities identified in the research.
Additionally, this research plays a crucial role in understanding how socio-demographic factors contribute to health outcomes. The data revealed patterns related to age, income, and educational levels that correlated with incidences of cancer and treatment accessibility. Insights drawn from this analysis will serve to not only pinpoint areas in need of support but also inform the development of culturally sensitive care approaches that consider diverse populations and their unique healthcare needs.
This study is particularly timely in light of ongoing discussions about healthcare reform globally. As nations grapple with how to address healthcare accessibility, the methodologies employed by the ONCOnnect consortium may serve as a model for similar initiatives worldwide. The intersection of technology, healthcare data, and community engagement is proving to be an essential pathway to achieving equitable access.
Moreover, the integration of geographic data in healthcare mapping signifies a paradigm shift in how medical services can be optimized and tailored. It transcends traditional boundaries, encouraging a more holistic approach to patient care. By embracing technology and advanced data analytics, healthcare systems can redefine their strategies and ultimately reshape the patient experience.
In conclusion, the comprehensive analysis conducted by the ONCOnnect consortium represents a substantial leap forward in understanding, evaluating, and ultimately enhancing cancer care accessibility in Germany. The combination of geographic data with healthcare insights offers a powerful tool to challenge existing disparities and advocate for a more equitable healthcare landscape. As the data continues to be analyzed and debated, the implications of this research will echo into future policy decisions, shaping the narrative of cancer care for years to come.
The collaborative efforts of this research team not only stand to improve outcomes for cancer patients but also serve as an inspiration for other nations confronting similar healthcare challenges. Through the innovative merging of data and a steadfast commitment to patient well-being, the ONCOnnect initiative paves the way for a brighter, more accessible future in cancer care.
Subject of Research: Geographic analysis of cancer care access in Germany
Article Title: Assessing the catchment area of German comprehensive cancer centers by merging geographic healthcare data – an initiative of the ONCOnnect consortium
Article References:
Kerscher, A., Metzler, M., Kapitza, J. et al. Assessing the catchment area of German comprehensive cancer centers by merging geographic healthcare data – an initiative of the ONCOnnect consortium. J Cancer Res Clin Oncol 151, 250 (2025). https://doi.org/10.1007/s00432-025-06272-0
Image Credits: AI Generated
DOI: 10.1007/s00432-025-06272-0
Keywords: cancer care, healthcare accessibility, geographic information systems, ONCOnnect consortium, health data analysis, disparities in healthcare