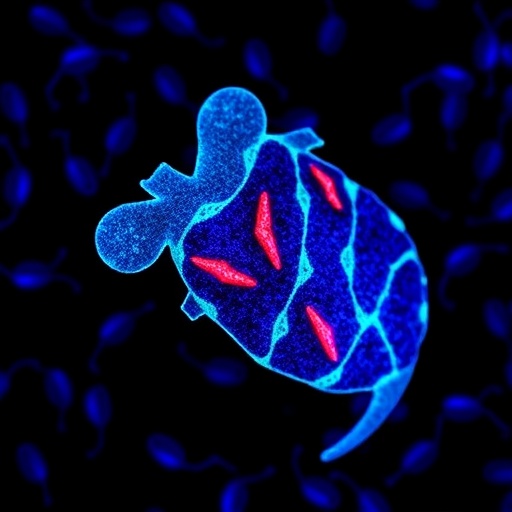
In a groundbreaking study that sheds light on innovative cardiac therapies, researchers have unveiled a novel approach to treating right ventricular dysfunction. This study, led by Watanabe et al., focuses on the creation and application of patches derived from human induced pluripotent stem cell (iPSC)-derived cardiomyocytes, marking a significant leap forward in regenerative medicine.
The heart, a vital organ, relies on the proper functioning of its chambers to maintain efficient blood circulation throughout the body. However, various conditions can lead to right ventricular hypertrophy and subsequent dysfunction. This is particularly prevalent in diseases such as pulmonary hypertension and congenital heart defects. Traditional treatments often fall short, prompting the need for advanced therapies that can restore heart function more effectively.
To address this pressing issue, the researchers utilized human pluripotent stem cells, which have the remarkable ability to differentiate into various cell types, including cardiomyocytes. By isolating these stem cells and directing their development toward cardiac cells, researchers created functional patches that can be implanted into the heart tissue. This innovative technique aims not only to repair but also to enhance the overall functionality of the right ventricle.
In experiments involving a rat model with pressure-overloaded right ventricles, the scientists applied these cardiomyocyte patches to assess their impact on heart function. The results were promising. The patches not only integrated well into the existing cardiac tissue, but they also demonstrated supportive effects on the overall health of the heart by improving hemodynamic parameters. This suggests that cell therapies could represent a pivotal shift in the treatment paradigm for patients suffering from right heart dysfunction.
The biocompatibility of the patches was a crucial aspect of the study. The research team ensured that the iPSC-derived cardiomyocytes exhibited characteristics similar to native cardiac cells, reducing the risk of rejection when implanted. Furthermore, they monitored the inflammatory response post-implantation, which is essential to ascertain whether the body could accept the foreign cellular material without adverse effects.
One of the remarkable outcomes of this research is the regulation of the extracellular matrix (ECM) surrounding the cardiomyocytes within the patches. The ECM plays a vital role in supporting cell structure and function, and in this study, it was found that the patches could positively modify the heart’s microenvironment. This augmentation is noteworthy because it could foster better integration of the patches with the host tissue, leading to improved repair and regeneration of the damaged myocardium.
Another critical element of this research is the mechanistic understanding of how these engineered patches facilitate enhancement in ventricle performance. The study revealed that the patches appeared to stimulate the endogenous cardiac repair processes, promoting the survival of host cardiomyocytes and potentially enhancing their contractile function. This could open doors to new therapeutic strategies that go beyond mere patching of tissues.
As the research progresses, the implications of using iPSC-derived therapies in clinical settings gain importance. The potential for creating patient-specific patches reduces the risks associated with donor tissue use, including ethical considerations and complications arising from immunogenic responses. This advance could lead to significant cost reductions in long-term care, while also improving patients’ quality of life.
Further studies are essential to assess the long-term efficacy and safety of these cardiomyocyte patches in larger animal models before transitioning to human trials. There is also an urgent need to refine the techniques used for differentiating iPSCs into cardiomyocytes, optimizing patch design, and assessing biomechanical properties to ensure they can withstand the dynamic environment of the heart.
In conclusion, Watanabe et al.’s research marks a significant milestone in cardiac regenerative medicine. It underscores the potential of iPSC technology in developing novel therapeutic strategies that could transform the approach to treating right ventricular dysfunction. This study not only paves the way for future research endeavors but also rekindles hope for patients battling chronic heart conditions, driving the scientific community toward a future where heart regeneration could become a standard practice.
The findings from this research are anticipated to stimulate further investigations into cell-based therapies, encouraging the exploration of various other cell types and their potential applications in regenerative medicine. The journey from bench to bedside is always complex, but the promise embodied in these cardiomyocyte patches is capturing researchers’ and clinicians’ imaginations alike.
The integration of technology and biology in creating solutions for one of the most critical organs in the body is an exciting frontier in medicine. The prospects of harnessing the body’s own regenerative capabilities through engineered tissues could well lead to a more resilient era in healthcare, emphasizing the need for continued investment in such transformative research endeavors.
As the world awaits the next steps in this promising research domain, the ripple effects of this study emphasize a broader vision in which personalized medicine, tissue engineering, and regenerative strategies converge, representing a beacon of hope for millions grappling with heart diseases.
Subject of Research:
Cardiac Regenerative Medicine Using Human Induced Pluripotent Stem Cells
Article Title:
Human induced pluripotent stem cell-derived cardiomyocyte patches ameliorate right ventricular function in a rat pressure-overloaded right ventricle model.
Article References:
Watanabe, T., Kawamura, T., Harada, A. et al. Human induced pluripotent stem cell-derived cardiomyocyte patches ameliorate right ventricular function in a rat pressure-overloaded right ventricle model. J Artif Organs 28, 234–243 (2025). https://doi.org/10.1007/s10047-024-01479-3
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s10047-024-01479-3
Keywords: Cardiomyocytes, Induced Pluripotent Stem Cells, Regenerative Medicine, Right Ventricular Dysfunction, Hemodynamics, Extracellular Matrix, Tissue Engineering, Biocompatibility.