In a groundbreaking two-center study published in BMC Cancer, researchers have unveiled a novel approach that harnesses the power of deep learning (DL) combined with advanced multiparametric MRI (mpMRI)-based habitat analysis to predict perineural invasion (PNI) in prostate cancer (PCa). This innovative method marks a significant stride in oncological imaging, potentially revolutionizing the way clinicians assess tumor behavior and insurance prognosis with striking accuracy.
Perineural invasion, the process by which cancer cells infiltrate the nerves surrounding a tumor, is a critical biomarker linked to aggressive disease progression and poor outcomes in prostate cancer patients. Traditionally, detecting PNI has relied heavily on invasive biopsy procedures and pathological examination, which come with limitations in sensitivity and spatial accuracy. Addressing these challenges, the study pivots toward a non-invasive imaging strategy, leveraging mpMRI to capture intricate tumor heterogeneity and generate quantifiable biomarkers predictive of PNI.
The research incorporated a substantial retrospective cohort of 397 prostate cancer patients recruited from two distinct medical centers, enabling a robust evaluation across diverse clinical settings. These patients were segmented into three distinct groups: a training cohort of 173 individuals, an internal validation (in-vad) group of 74, and an external validation (ex-vad) cohort consisting of 150 patients. This structured division ensured rigorous model training and unbiased assessment of predictive capability.
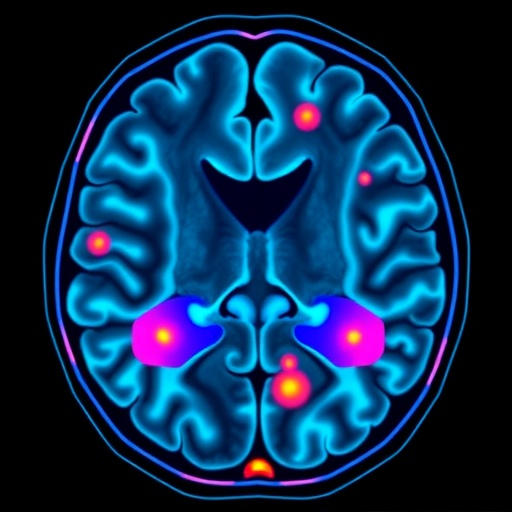
At the core of this study lies the concept of habitat analysis, a technique devised to dissect the tumor microenvironment into spatially distinct “habitats” by integrating key mpMRI sequences — specifically, T2-weighted imaging (T2WI), diffusion-weighted imaging (DWI), and apparent diffusion coefficient (ADC) maps. This multiparametric fusion elucidates differing tissue characteristics within the tumor mass, such as variations in cellularity and extracellular matrix composition, that are otherwise imperceptible through conventional imaging alone.
Following habitat segmentation, the study applied a tailored deep learning framework to extract complex features from these subregions. Through a meticulous feature selection and filtration process, the researchers derived a composite score termed “radscore.” This radscore effectively encapsulates the heterogeneity-driven imaging biomarkers that correlate with the presence or absence of perineural invasion.
The investigative team constructed six predictive models to compare and optimize PNI detection. These included a purely clinical model based on conventional patient data, four habitat-specific models addressing individual tumor subregions, and a combined model merging clinical parameters with mpMRI-derived radiomics. The overarching goal was to ascertain which approach delivered the highest discriminative power.
Results from receiver operating characteristic (ROC) curve analysis were remarkable. The four habitat models exhibited formidable performance across all cohorts, with area under the curve (AUC) values ranging between 0.802 and 0.957. This high degree of accuracy underscores the utility of habitat-specific imaging markers in capturing the nuanced biology of perineural invasion.
The standalone clinical model, while informative, demonstrated relatively modest performance with AUCs of 0.832, 0.818, and 0.789 in the training, internal validation, and external validation sets, respectively. This gap highlighted the necessity of integrating imaging biomarkers with classic clinical data to achieve superior predictive fidelity.
Most notably, the combined model, which synthesized clinical data and habitat-based radiomic features, substantially outperformed all other models. In the training cohort, this integrated approach attained an exceptional AUC of 0.999, alongside near-perfect sensitivity and specificity of 1 and 0.955, respectively. Such precision indicates that the combined model could virtually eliminate false negatives and false positives, addressing a critical unmet need in prostate oncology diagnostics.
Further substantiating the clinical relevance, decision curve analysis (DCA) and clinical impact curve analysis demonstrated that the combined model offers tangible benefits in patient management decisions. This implies that incorporating this predictive tool in routine workflow could guide more personalized treatment planning, reduce unnecessary interventions, and potentially improve patient outcomes.
The significance of these findings is multi-dimensional. Firstly, this study exemplifies how quantitative imaging biomarkers, when paired with cutting-edge artificial intelligence, can transform subjective radiological evaluation into objective and reproducible diagnostics. The deployment of mpMRI-based habitat analysis offers a window into tumor microenvironment traits that are pivotal for understanding cancer aggressiveness.
Secondly, the use of deep learning pipelines enables the extraction of high-dimensional, non-linear features from imaging data that elude traditional radiomics and human interpretation. The radscore concept epitomizes this integration, proving that sophisticated computational methods can condense complex imaging phenotypes into actionable clinical predictors.
Moreover, this research sets a precedent for multi-institutional collaboration, validating the generalizability of imaging-based predictive models across heterogeneous patient populations and clinical settings. The use of an external validation cohort fortifies confidence that these findings are not confined to a single center’s imaging protocols or patient demographics.
Despite the triumphs, the investigators acknowledge that further prospective studies are warranted to evaluate the model’s performance in real-time clinical scenarios and to integrate it with emerging biomarkers such as genomic or proteomic data. Additionally, prospective trials could assess the impact of this predictive approach on therapeutic decision-making and long-term patient survival.
The promise of DL and habitat analysis also extends beyond prostate cancer, potentially catalyzing analogous advances in other solid tumors where perineural invasion and tumor heterogeneity profoundly influence prognosis. As imaging technology and computational models continue to evolve, such integrated tools will become indispensable in precision oncology.
In essence, this pioneering study illuminates a path toward non-invasive, accurate, and clinically actionable prediction of perineural invasion in prostate cancer. The alignment of multiparametric MRI, habitat analysis, and deep learning heralds a new era of imaging biomarker discovery, promising to enhance diagnostic confidence and ultimately reshape patient care paradigms in urologic oncology.
Subject of Research: Prediction of perineural invasion in prostate cancer using multiparametric MRI-based habitat analysis and deep learning.
Article Title: A novel MRI-based habitat analysis and deep learning for predicting perineural invasion in prostate cancer: a two-center study
Article References:
Deng, S., Huang, D., Han, X. et al. A novel MRI-based habitat analysis and deep learning for predicting perineural invasion in prostate cancer: a two-center study. BMC Cancer 25, 1367 (2025). https://doi.org/10.1186/s12885-025-14759-9
Image Credits: Scienmag.com