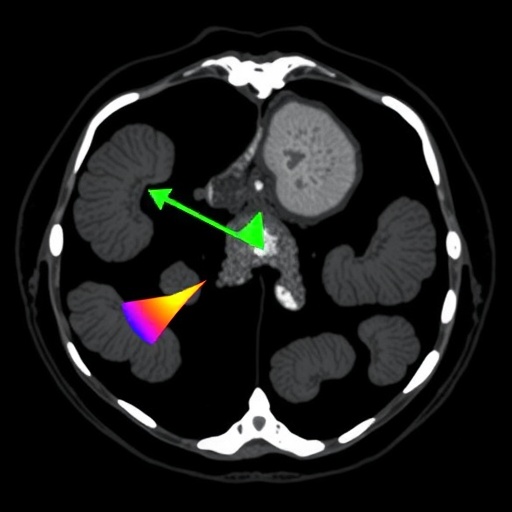
In a groundbreaking advancement poised to transform emergency obstetric care, researchers from Kumamoto University have identified a distinctive and diagnostically powerful imaging marker on dynamic computed tomography (CT) scans that predicts the severity of postpartum hemorrhage (PPH) and the necessity for life-saving interventions such as uterine artery embolization. This novel CT imaging signature, termed PRACE—an acronym for Postpartum hemorrhage, Resistance to treatment, and Arterial Contrast Extravasation—introduces a paradigm shift in how clinicians evaluate and manage one of the leading causes of maternal mortality worldwide.
Postpartum hemorrhage remains a formidable challenge in obstetrics, accounting for a significant proportion of maternal deaths despite advances in medical care. Most instances respond effectively to uterotonics and straightforward clinical interventions; however, a critical subset of patients experiences relentless, severe bleeding that resists conventional treatment modalities, substantially increasing risk of fatal outcomes. Until now, clinicians have lacked reliable diagnostic tools to stratify risk dynamically and determine early which patients require invasive treatments such as uterine artery embolization (UAE).
The nationwide study, conducted across 43 premier medical institutions in Japan, analyzed 352 cases of severe postpartum bleeding, with 205 patients subjected to dynamic CT scans to investigate vascular patterns associated with hemorrhage progression. Remarkably, 58 of these cases, representing over 30%, exhibited the distinct PRACE pattern characterized by active extravasation of contrast agent into the uterine cavity during the early imaging phase, signaling ongoing arterial bleeding that defied pharmacological suppression.
Statistical analyses underscored the predictive power of PRACE: patients displaying this pattern were more than three times as likely to necessitate UAE compared to those without it, with incidence rates of 86.2% versus 28.7%, respectively. Beyond the correlation with interventional requirements, the PRACE-positive group also demonstrated a higher prevalence of coagulopathy, compromising physiological hemostasis, and frequently required substantial blood transfusions to stabilize hemodynamics. The odds ratio calculated for the need of embolization in presence of PRACE reached an unprecedented 27.74, establishing this imaging biomarker as the most potent predictor of clinical escalation identified to date.
Dynamic CT imaging involves administering iodinated contrast material and capturing rapid-sequence images to visualize vascular perfusion and potential leakage points in real time. The ability to detect arterial contrast extravasation early offers a decisive advantage in identifying ongoing, uncontrolled bleeding before it manifests clinically. This early warning enables prompt deployment of uterine artery embolization—a minimally invasive endovascular technique that occludes hemorrhaging vessels—thus averting deterioration and preserving maternal lives.
Professor Eiji Kondoh of Kumamoto University’s Faculty of Life Sciences emphasized the transformative potential of PRACE, describing it as “a game-changer in how we assess and respond to critical postpartum bleeding.” He elaborated that incorporation of dynamic CT in emergency obstetric protocols not only enhances diagnostic accuracy but also revolutionizes clinical workflows, shifting the approach from reactive to proactive. This technique empowers caregivers to stratify hemorrhage risk dynamically and tailor interventions with precision.
The researchers propose expanding the conventional “4 Ts” framework used to categorize PPH causes—Tone, Trauma, Tissue, and Thrombin—by adding a fifth dimension reflecting CT imaging findings. By integrating PRACE and similar imaging biomarkers, clinicians can refine risk stratification, prioritizing patients for advanced management and optimizing resource allocation during critical care scenarios. This evolution signifies a decisive leap toward precision medicine in maternal health.
Despite the undeniable promise, dynamic CT usage in acute postpartum settings necessitates balancing benefits against exposure risks, particularly radiation and contrast-induced nephropathy. The researchers advocate for judicious application in high-risk cases where traditional assessment tools fall short, underscoring that careful patient selection and optimized imaging protocols can mitigate such concerns. Subsequent work is anticipated to refine criteria for CT utilization and to integrate artificial intelligence to automate and accelerate image interpretation.
Complementing imaging findings, the study’s robust statistical framework incorporated multivariate analyses that controlled for confounding variables such as age, parity, and co-existing medical conditions. This methodological rigor strengthens confidence in PRACE’s independence as a prognostic indicator. Additionally, translational insights suggest that arterial contrast extravasation visualized through dynamic CT aligns pathophysiologically with persistent arterial injury or erosion unresponsive to vasoconstrictive medications, corroborating clinical observations.
The impact of these findings extends beyond Japan, holding global relevance for obstetric practice. As PPH remains a major contributor to maternal morbidity in both low- and high-resource settings, integrating advanced imaging technology could bridge gaps in timely diagnosis and intervention. Nevertheless, implementation challenges such as equipment availability, training, and workflow integration must be addressed to realize full clinical benefits universally.
Moreover, the study opens avenues for future innovation, including real-time bedside imaging and hybrid techniques combining ultrasonography with CT-derived risk parameters. Such integrative diagnostics could further enhance the sensitivity and specificity of hemorrhage severity assessments, fostering multidisciplinary care strategies that unite radiologists, obstetricians, and interventional specialists in cohesive response teams.
In summary, the identification of dynamic CT’s PRACE pattern marks a significant milestone in the battle against life-threatening postpartum hemorrhage. By revealing occult arterial bleeding resistant to conventional therapy, this imaging biomarker provides an invaluable tool for early intervention, optimizing maternal outcomes and potentially saving countless lives. The work of Kumamoto University researchers thereby charts a bold course toward reshaping obstetric emergency care in the 21st century.
Subject of Research: People
Article Title: Dynamic Computed Tomography Findings as Indicators of Uterine Artery Embolization in Postpartum Hemorrhage
News Publication Date: 23-May-2025
Web References:
http://dx.doi.org/10.1001/jamanetworkopen.2025.12209
Image Credits:
Yamaguchi et al.
Keywords:
Bleeding, Clinical imaging, Clinical studies, Medical treatments, Blood transfusion, Uterus, Arteries, Childbirth, Odds ratios, Pathology, Diagnostic accuracy