In the rapidly evolving field of adolescent mental health, a groundbreaking study has emerged that intricately maps the complex web of cognitive, emotional, and pain perception factors tied to non-suicidal self-injury (NSSI) among Chinese adolescents. Published in BMC Psychology, this 2025 study spearheaded by Luo, Gong, Zhou, and colleagues offers a novel network-based understanding, shedding unprecedented light on how internal psychological states and sensory experiences intertwine in this vulnerable population. As rates of NSSI continue to alarm clinicians and researchers worldwide, particularly in East Asian contexts, this research breaks new ground by integrating diverse psychological constructs into a cohesive explanatory framework.
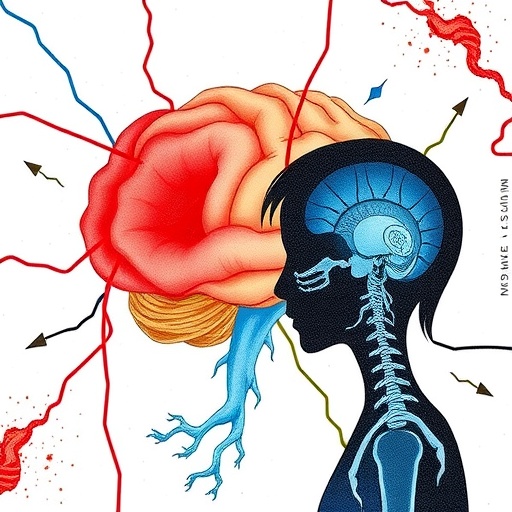
Non-suicidal self-injury, the deliberate harm inflicted on one’s body without suicidal intent, has perplexed specialists for decades due to its multifaceted nature. Historically, research perspectives focused on isolated factors such as depression, anxiety, or trauma. However, this innovative study moves beyond siloed analyses by constructing an interconnected network model that reveals how cognitive distortions, emotional dysregulation, and altered pain perception dynamically interact to influence self-injurious behaviors. The authors’ approach aligns with contemporary shifts towards viewing psychopathology as a complex system, rather than a collection of independent symptoms.
At the anatomical level, the study’s insights tap into emerging neuroscientific findings connecting brain regions involved in pain modulation, emotion regulation, and executive functioning. Adolescents engaging in NSSI often report atypical experiences of pain that both precede and follow self-injurious episodes. Luo and colleagues theorize that a dysregulated pain perception system may serve a dual role: dulling psychological distress through physical sensation, yet paradoxically reinforcing harmful behaviors through neurobiological reward mechanisms. This intricate balance between pain and relief is critical in understanding why traditional therapeutic strategies may fall short for many youths.
The cognitive domain, as examined in this research, elucidates patterns of maladaptive thinking that reinforce self-injury. Distorted appraisal mechanisms, such as catastrophizing negative emotions or pervasive feelings of helplessness, amplify emotional suffering. This mental framework lays the groundwork for subsequent compulsive self-harm as a maladaptive coping strategy to regain perceived control or to communicate internal anguish. Crucially, the network analysis highlights how these cognitive distortions connect bidirectionally with emotional and sensory pathways, forging a cyclical trap difficult for adolescents to escape without targeted intervention.
Emotional regulation emerges as a pivotal node in the network identified by the study. Adolescents prone to NSSI frequently exhibit reduced capacity to manage overwhelming affective states, ranging from intense sadness to irritability and numbness. The inability to modulate emotional intensity fuels the urgency to engage in self-injury as an immediate, though destructive, mode of relief. This study further delineates nuances within emotional processes by distinguishing between affective lability, alexithymia (difficulty identifying emotions), and trauma-related dysregulation, each contributing uniquely to the risk profile.
What sets this investigation apart is its cultural sensitivity and specificity. Previous Western-centric models often overlook socio-cultural factors influencing adolescent mental health. Conducted in China, this research contextualizes findings within societal pressures and stigma surrounding mental illness and help-seeking behaviors. It draws attention to the silent epidemic of self-injury exacerbated by academic stress, family expectations, and rapid socio-economic changes, which uniquely shape Chinese youth experiences. Such contextual depth enhances the applicability of findings for both local clinical practice and global comparative studies.
Methodologically, the study utilizes advanced statistical modeling techniques known as network psychometrics, where symptoms and psychological constructs are treated as interconnected “nodes” rather than isolated variables. This allows for visualization of how tightly clusters of factors co-occur and influence one another dynamically. Notably, certain nodes, such as emotional dysregulation and pain sensitivity, demonstrate high centrality, indicating their critical influence within the network and positioning them as prime therapeutic targets. This precise mapping signifies a leap towards personalized or precision mental health care.
The relationship between pain perception and emotional distress uncovered here also resonates with the neurobiological concepts of endogenous opioid function and stress-induced analgesia. Adolescents displaying altered pain thresholds might be experiencing dysregulated endogenous pain inhibition systems, which in turn exacerbate emotional turmoil. This biobehavioral feedback loop forms a self-sustaining pattern, often escaping detection in conventional psychiatric evaluations focused primarily on symptom reduction rather than mechanistic understanding.
Moreover, the study’s longitudinal design, following participants over an extended timeframe, permits observation of temporal changes and causal hypotheses. While cross-sectional studies offer snapshots, this dynamic approach captures the ebb and flow of cognitive-emotional-pain networks as adolescents develop and as interventions are introduced. Early findings suggest that interventions targeting emotional regulation skills may disrupt the reinforcing cycles of self-injury more effectively than strategies focusing solely on mood symptoms.
From a clinical perspective, this research advocates for integrative intervention frameworks combining cognitive-behavioral therapy with somatosensory and emotion-focused components. Techniques such as dialectical behavior therapy (DBT), mindfulness-based stress reduction, and pain modulation therapies may be synergistically employed. The nuanced characterization of network nodes also informs screening procedures, emphasizing the need to assess pain perception anomalies alongside traditional mental health symptoms during routine adolescent evaluations.
Public health implications are equally profound. With rising awareness of adolescent NSSI driven partly by social media exposure and pandemic-era isolation, the identification of key psychological mechanisms underpinning self-injury could inform preventive programs at schools and community levels. Educational campaigns leveraging this scientific knowledge could destigmatize emotional struggles and normalize discussions around pain experiences and coping methods, reducing the risk of covert self-injury.
Ethically, this study raises important questions on balancing research advancement with respect for adolescent vulnerability. The authors’ meticulous attention to confidentiality, culturally appropriate consent procedures, and sensitive data interpretation underscores best practices for psychological research within diverse populations. Their approach models how complex mental health phenomena can be investigated without exacerbating stigma or triggering distress among participants, a crucial consideration given the sensitive topic of self-injury.
In the broader scope of neuroscience and psychology, the concept of interconnected symptom networks challenges traditional categorical diagnostic systems such as DSM or ICD. Instead, it favors dimensional and transdiagnostic models recognizing overlapping features across mental disorders. Luo and colleagues’ findings contribute valuable empirical evidence supporting this paradigm shift and encourage interdisciplinary collaboration to refine diagnostic criteria and treatment approaches accordingly.
Future directions indicated by the study include exploring genetic and epigenetic factors that might predispose individuals to the identified cognitive-emotional-pain network configurations. Additionally, integrating neuroimaging data could deepen mechanistic insights, linking structural and functional brain anomalies to behavioral presentations. Such advances would further bridge the gap between bench science and clinical therapeutics, paving the way for biomarker-assisted diagnoses and individualized treatment plans.
This pioneering work also invites research into ecological momentary assessment (EMA) methodologies deploying real-time mobile monitoring of mood, cognition, and pain symptoms. Capturing fluctuations outside laboratory or clinical settings enables a granular understanding of NSSI triggers and maintenance factors in naturalistic contexts. Real-time interventions via digital platforms could thereby be tailored dynamically, enhancing efficacy and adherence among tech-savvy adolescent populations.
In conclusion, the Luo et al. study represents a significant stride toward unraveling the tangled psychological and neurobiological networks underpinning non-suicidal self-injury in Chinese adolescents. By integrating cognitive distortions, emotional dysregulation, and pain perception into a sophisticated network model, the research not only advances scientific understanding but also charts promising paths for innovative treatments and preventive efforts. Its culturally attuned, methodologically rigorous, and clinically relevant insights offer a beacon of hope in the challenging quest to support vulnerable youth navigating the complex terrain of self-harm.
Subject of Research: Network analysis of cognitive, emotional, and pain perception factors associated with non-suicidal self-injury (NSSI) in Chinese adolescents.
Article Title: Network of cognitive, emotional, and pain perception factors linked to non-suicidal self-injury in Chinese adolescents.
Article References:
Luo, W., Gong, J., Zhou, Hy. et al. Network of cognitive, emotional, and pain perception factors linked to non-suicidal self-injury in Chinese adolescents.
BMC Psychol 13, 933 (2025). https://doi.org/10.1186/s40359-025-03296-6
Image Credits: AI Generated