Rhabdomyosarcoma, a malignancy predominantly affecting children and adolescents, has long posed significant challenges in oncology. This soft tissue sarcoma can be particularly aggressive, prompting the medical community to seek out effective treatment modalities. A recent study published in Pediatric Radiology sheds light on the relationship between early radiologic tumor volume response and overall survival rates in patients with non-metastatic rhabdomyosarcoma. This study raises compelling questions about current prognostic strategies and their implications for future clinical practices.
Traditionally, clinicians have relied on early tumor volume response as a vital indicator of long-term survival in cancer therapies. The assumption was that a substantial reduction in tumor size shortly after treatment initiation could serve as a proxy for better outcomes. However, this notion has not always been empirically substantiated across various types of cancers, particularly in pediatric populations where the disease behavior may differ markedly from adults. The study by de Vries et al. calls this assumption into question, demonstrating that such early responses may not reliably predict survival for children with rhabdomyosarcoma.
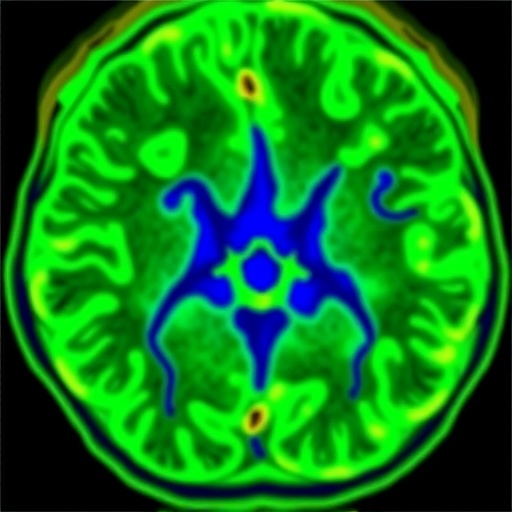
The researchers conducted a comprehensive analysis involving a prospective cohort of patients diagnosed with non-metastatic rhabdomyosarcoma. They meticulously monitored these patients’ tumor responses through advanced imaging techniques, assessing changes in tumor volume over a defined treatment duration. This approach underscores the increasing importance of high-resolution radiologic assessments in understanding tumor dynamics and patient prognosis.
In their findings, de Vries and colleagues reported that despite favorable initial tumor responses to treatment, this did not correspond with improved survival outcomes. This paradox raises critical questions about the efficacy of current treatment protocols and calls for a reevaluation of how we gauge success in treating this condition. The implications extend beyond immediate clinical practices; these revelations may also inform the development of future therapeutic strategies.
The study employed a range of imaging modalities to track tumor responses. Techniques such as MRI and CT scans were utilized to assess volumetric changes with precise accuracy, allowing researchers to capture the nuances of tumor behavior over time. This detailed imaging represents a significant advancement over previous methodologies that relied solely on qualitative assessments or solitary size measurements, thereby providing a more comprehensive understanding of tumor biology.
Understanding why early tumor volume response does not correlate with survival requires deeper insight into the biochemistry and cellular mechanisms underlying rhabdomyosarcoma. Indeed, tumor biology is known to be incredibly complex; it involves a myriad of genetic alterations and microenvironmental factors that may dictate a tumor’s behavior independent of size alone. The findings suggest that less emphasis should be placed on early volumetric response metrics in the prognostic equation, prompting the need for alternative biomarkers that could more accurately reflect underlying disease processes.
The implications of this study for clinical practice are substantial. If radiologic tumor volume response is not a reliable indicator of survival, oncologists may need to adopt a more nuanced approach to treatment planning, possibly focusing on a combination of factors, including patient age, tumor genetics, and other clinical characteristics. This holistic view could enhance personalized medicine efforts in the realm of pediatric oncology, ultimately paving the way for tailored treatment protocols that consider the diverse interactions within tumor biology.
Furthermore, these findings challenge the notion of early intervention as a panacea for cancer treatments. While early treatment may still be critical, the metrics by which we measure success need significant refinement. As our understanding of cancer deepens through ongoing research, it becomes increasingly clear that simplistic correlations between treatment response and survival may overlook critical complexities intrinsic to tumor behavior.
Additionally, this study denotes a paradigm shift in how we address prognostication in pediatric cancers. It prompts further inquiry into alternative methods, potentially bringing forward new technologies or biochemical markers that could give a clearer picture of patient outcomes than traditional imaging alone. The quest continues for reliable prognostic indicators that can support clinicians in making informed decisions about treatment adaptations in real time.
This pivotal research opens avenues for further investigation into non-invasive measures that could supplement traditional imaging, such as liquid biopsies or biologic markers representing tumor activity at the molecular level. As we continue to unravel the intricacies of rhabdomyosarcoma, this exploration could yield invaluable insights into more effective treatment modalities and better patient care strategies.
In summary, the work published by de Vries et al. serves as a critical reminder of the limits of current prognostic indicators in pediatric oncology. By challenging the efficacy of transient tumor volume changes as predictors of survival, the study presents an opportunity for reframing our approaches to cancer treatment and management, steering the profession toward a future of precision medicine where outcomes can be anticipated with greater accuracy.
Notably, these findings resonate with a broader movement within oncology to critically evaluate established treatment paradigms. As research evolves, the findings of today could catalyze the breakthroughs of tomorrow, ultimately transforming the landscape of cancer treatment for future generations.
In conclusion, the study marks a significant step in enhancing our understanding of rhabdomyosarcoma and emphasizes the necessity for continuous innovation and exploration in pediatric cancer treatment. The quest for more reliable prognostic measures is not just a scientific endeavor; it has profound implications for the lives of patients and their families.
Subject of Research: Prognostic Indicators in Rhabdomyosarcoma
Article Title: Early radiologic tumour volume response in non-metastatic rhabdomyosarcoma is not predictive for survival.
Article References: de Vries, I., Morosi, C., Bisogno, G. et al. Early radiologic tumour volume response in non-metastatic rhabdomyosarcoma is not predictive for survival. Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06359-3
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00247-025-06359-3
Keywords: Rhabdomyosarcoma, Tumor Volume, Prognosis, Pediatric Oncology, Radiology.