In the United States, cervical cancer remains a significant public health challenge, particularly in regions marked by socio-economic disparities and healthcare access limitations. Recent research conducted by scientists at the MUSC Hollings Cancer Center reveals a powerful correlation between county-level cervical cancer screening rates and the incidence as well as mortality rates associated with the disease. This comprehensive analysis, recently published in JAMA Network Open, delineates how counties with persistently low screening rates suffer disproportionately higher burdens of cervical cancer diagnoses and deaths, underscoring the urgent need for enhanced preventive healthcare strategies targeted at these vulnerable communities.
Dr. Trisha Amboree, Ph.D., a leading epidemiologist involved in the study, highlights that cervical cancer outcomes are intricately tied to screening practices. Prior work from the MUSC team established that incidence and mortality for cervical cancer escalate significantly in rural and low-income U.S. counties, but the underlying causative factors were not fully elucidated. The new study advances this understanding by leveraging extensive county-level screening data spanning over a decade to investigate how differential screening coverage impacts cancer occurrence and fatality rates.
The absence of a unified national cervical cancer screening registry in the United States presents a formidable obstacle to directly linking individual screening histories with cancer outcomes. To circumvent this limitation, the research team employed county-level screening metrics as proxies to assess the broader epidemiological patterns reflecting prevention efficacy. This ecological approach, while lacking granular individual data, permits robust statistical associations revealing that consistently low screening rates notably drive increased disease burdens.
Screening for cervical cancer primarily involves Pap smear cytology and human papillomavirus (HPV) testing—both of which serve as vital tools for early detection and intervention. The biological rationale for widespread screening is the identification of precancerous cervical lesions amenable to removal before malignant transformation occurs. Furthermore, timely screening facilitates diagnosis at earlier cancer stages, significantly improving treatment outcomes and survival probabilities. These established clinical benefits underpin national screening guidelines advocating regular testing intervals for women within specified age brackets.
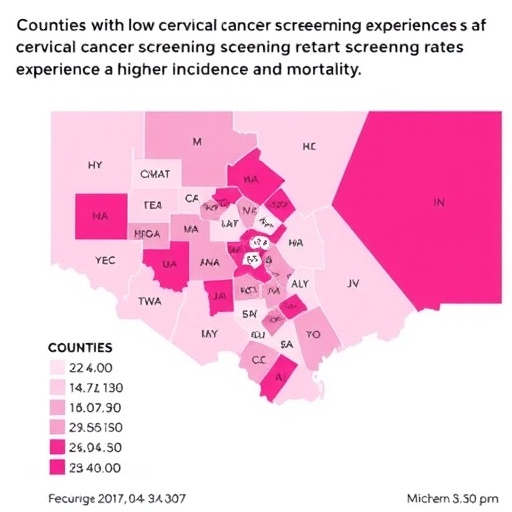
Within the analyzed data collected between 2004 and 2016, counties were categorized based on screening prevalence: those with fewer than 70% of eligible women screened in at least two of three defined time periods were labeled as “repeatedly low-screening,” while counties with at least 80% screening coverage earned the “repeatedly high-screening” designation. The national cervical cancer screening benchmark is set at 79.2%, framing these categorizations within the context of public health goals.
The comparative findings between these two groups revealed striking disparities. Counties labeled as repeatedly low-screening exhibited an 84% higher incidence of distant-stage cervical cancer when contrasted with their high-screening counterparts. Even more concerning was the 96% increase in cervical cancer mortality within the low-screening counties. These statistics not only reaffirm the protective effect of routine screenings but also illuminate how persistent under-screening directly correlates with worsened clinical outcomes.
An important demographic pattern emerged from the data analysis—the vast majority of low-screening counties were rural, and all shared an annual median household income below $75,000. This intersection of geographic isolation and economic disadvantage likely contributes to reduced access to gynecological services, educational resources, and preventive healthcare measures. Indeed, these socioeconomic constraints reinforce cancer health inequities and complicate public health intervention efforts.
The implications of these findings call for immediate and strategic responses to enhance cervical cancer screening accessibility and uptake, especially in rural and low-income communities. Increasing availability of screening services via mobile health clinics, like the one operated by MUSC Hollings Cancer Center, represents a promising model. These outreach initiatives mitigate barriers such as geographical distance and provider shortages, delivering essential preventive care directly to underserved populations.
Despite the comprehensive national scope of the study, data from South Carolina were not included in the assessed database. Nevertheless, Dr. Amboree posits that the state’s rural counties likely mirror the identified national trends. South Carolina faces its own physician shortages in gynecology and family medicine, with some counties lacking any obstetrician-gynecologists and others maintaining only minimal family practice coverage, further justifying localized efforts like Hollings’ Mobile Health Unit to bridge preventive care gaps.
Current recommendations from the U.S. Preventive Services Task Force guide cervical cancer screening protocols within the U.S. healthcare system. Women aged 21 to 65 are advised to undergo Pap smears every three years, whereas those aged 30 to 65 have the option of HPV testing, either alone or in combination with Pap testing, every five years. Adhering to these guidelines ensures timely detection while balancing the minimization of unnecessary procedures.
This study serves as an urgent call to public health stakeholders to prioritize cervical cancer screening programs’ expansion and affordability, particularly for hard-to-reach populations. Through coordinated efforts encompassing policy initiatives, community education, and healthcare resource allocation, the reducible morbidity and mortality from cervical cancer can be curtailed. Such measures are vital to address the stark disparities highlighted by Dr. Amboree and colleagues, ultimately enhancing health equity and outcomes nationwide.
MUSC Hollings Cancer Center embodies a beacon for cancer research and clinical care in South Carolina. As the only National Cancer Institute-designated cancer center in the state, its extensive faculty and multidisciplinary expertise underpin significant contributions to cancer prevention, diagnosis, and treatment. Beyond clinical services, the center actively engages in community outreach and health education, emphasizing its commitment to reducing the cancer burden through evidence-based strategies and accessible interventions.
The compelling quantitative linkage established in this research between screening coverage and cervical cancer outcomes adds critical evidence for healthcare policymakers and practitioners advocating for sustained investment in cervical cancer prevention. It underscores the indispensable role of systematic screening as a frontline defense, particularly in socioeconomically disadvantaged and rural regions disproportionately afflicted by disease.
Ultimately, decreasing cervical cancer incidence and mortality requires a multipronged approach that integrates rigorous epidemiological surveillance, enhanced screening infrastructure, and targeted community engagement. Leveraging data-driven insights fortifies the foundation for tailored interventions designed to close existing care gaps and promote healthier futures for all women, regardless of geographic or economic status.
Subject of Research: County-level cervical cancer screening coverage and its association with differences in cervical cancer incidence and mortality rates.
Article Title: County-Level Cervical Cancer Screening Coverage and Differences in Incidence and Mortality
News Publication Date: 13-Aug-2025
Web References:
10.1001/jamanetworkopen.2025.26709
Image Credits: MUSC Hollings Cancer Center
Keywords: Cervical cancer, Public health, Rural populations