In recent years, the field of pediatric radiology has witnessed significant advancements, particularly in the imaging of acute injuries sustained during blunt thoracic trauma. This issue is of paramount importance, as children are uniquely vulnerable to such injuries due to their developing physiology. The review by Orscheln, Sandhu, and Shet delves into the complexities of diagnosing and managing these injuries, emphasizing the essential role of imaging techniques in successful outcomes.
Blunt thoracic trauma can arise from a multitude of scenarios, such as motor vehicle accidents, sports injuries, or falls. Each incident type presents its own challenges and necessitates different imaging modalities for appropriate assessment. The anatomical makeup of children complicates matters further due to differences in rib cage structure and the unique elasticity of their thoracic walls compared to adults. This has led researchers and clinicians to refine their approaches to imaging in this vulnerable population.
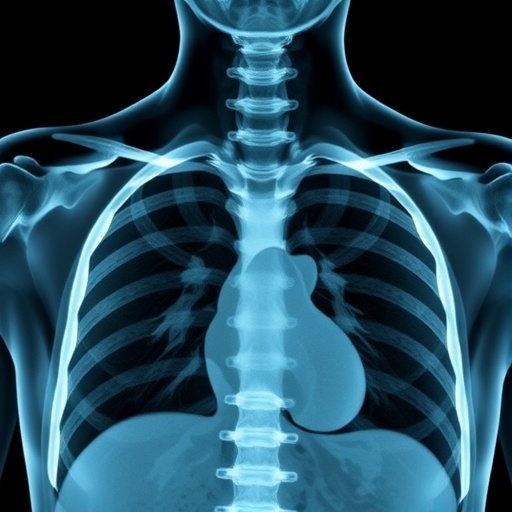
The choice of imaging modality is crucial. X-rays have been the traditional first-line investigation in trauma cases due to their speed and availability. However, their limitations in detecting subtle injuries can often lead to missed diagnoses. The authors argue that while X-rays remain essential, they should be complemented by advanced modalities, such as ultrasound and, more prominently, computed tomography (CT), which can provide a more comprehensive evaluation of thoracic trauma.
Ultrasound is particularly useful in a pediatric setting, as it avoids radiation exposure—an important consideration in the pediatric population. While ultrasound can effectively evaluate pleural effusions or solid organ injuries, its utility in identifying thoracic injuries related to rib fractures remains limited. Educating pediatricians and emergency medicine physicians about the strengths and weaknesses of each imaging modality is a pivotal step toward improving care.
Computed tomography (CT) scanning has revolutionized the assessment of thoracic trauma. Its superior sensitivity allows for the detection of subtle parenchymal injuries, vascular compromise, and associated thoracic injuries that could otherwise go unnoticed. The authors stress that while CT scans offer detailed imaging, clinicians must weigh the benefits against potential risks, particularly in light of cumulative radiation exposure in children.
In parallel with image acquisition, interpretation plays a critical role in managing pediatric blunt thoracic trauma. The authors highlight the importance of a multi-disciplinary approach involving pediatric radiologists, emergency medicine professionals, and trauma surgeons. A collaborative, team-oriented environment fosters more accurate diagnoses and subsequently improves patient outcomes.
Furthermore, the article discusses the costs associated with different imaging strategies. While CT scans may appear more expensive upfront, the cost differences shrink when considering the potential for misdiagnosis or delayed treatment stemming from inadequate initial assessments. Fostering clearer communication between healthcare providers regarding the importance of appropriate imaging can ensure children receive timely and effective care.
The psychological impact of trauma on pediatric patients is another significant aspect discussed. Depending on the injury’s severity, patients may require ongoing support, and parents often struggle with fear and anxiety regarding their children’s health. Thus, open lines of communication with families, explaining diagnostic processes, and addressing concerns can alleviate some of this burden.
Emerging technologies, such as magnetic resonance imaging (MRI), are also addressed in the article. While MRI is not typically the first choice in acute settings due to longer acquisition times and susceptibility to patient motion, advancements in imaging technology are making it increasingly valuable for specific cases, particularly where soft tissue details matter. Continued research into the applications of MRI in pediatric trauma can further enhance the diagnostic landscape.
Moreover, the authors suggest that educators and training programs should place a significant focus on pediatric trauma imaging. By providing fellowships and specialized training in pediatric radiology, future clinicians can be better equipped to handle the unique challenges posed by this patient demographic. Incorporating exposure to multidisciplinary teams during residency can cultivate a deeper understanding of how various specialties interact in trauma management.
The review culminates with a call to action for improved guidelines on imaging protocols in pediatric blunt thoracic trauma. Developing clear, evidence-based recommendations could standardize practices and ensure optimal care across hospitals. By simplifying the decision-making process for clinicians, such guidelines would help reduce variability in patient management and improve outcomes everywhere.
As pediatric blunt thoracic trauma requires a unique blend of skills, knowledge, and technology, the role of imaging becomes even more critical. By harnessing the power of advanced imaging modalities, fostering teamwork, and promoting continuous education, medical professionals can ensure that even in the face of trauma, young patients receive the best care possible.
The implications of this research extend far beyond the immediate management of injuries. It sheds light on the continuous evolution of pediatric radiology and the importance of addressing the unique needs of children in trauma settings. The future holds exciting prospects, ensuring that advancements in imaging keep pace with the evolving landscape of pediatric healthcare needs.
In conclusion, the insights presented in this article represent a pivotal moment for improving outcomes in pediatric blunt thoracic trauma. With multidisciplinary collaboration, commitment to continuous education, and a proactive approach to imaging, the healthcare community is poised to enhance the standard of care for our most vulnerable patients.
Subject of Research: Imaging in pediatric blunt thoracic trauma
Article Title: Imaging in pediatric blunt thoracic trauma
Article References:
Orscheln, E., Sandhu, P. & Shet, N. Imaging in pediatric blunt thoracic trauma. Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06356-6
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00247-025-06356-6
Keywords: Pediatric radiology, blunt thoracic trauma, imaging modalities, computed tomography, ultrasound, multidisciplinary care, psychological impact, MRI, trauma management, healthcare education.