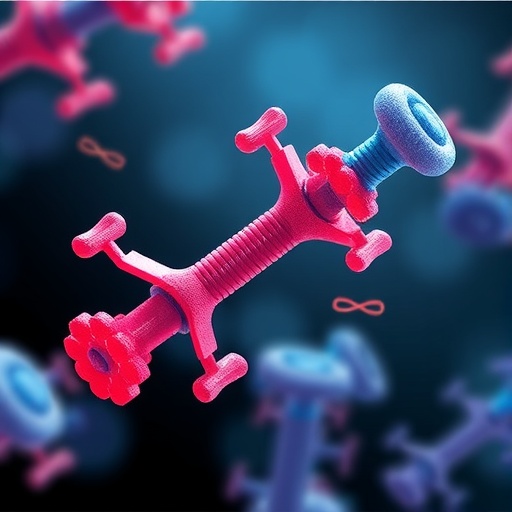
Antibody-Drug Conjugates (ADCs) represent a dynamic and rapidly evolving frontier in targeted cancer therapy, combining the specificity of monoclonal antibodies with the potent cytotoxic power of chemotherapeutic agents. This revolutionary therapeutic class aims to maximize tumor cell eradication while minimizing systemic toxicity, a delicate balance that continues to challenge oncologists and researchers alike. Recent developments, chronicled in a comprehensive review published in Protein & Cell, offer new insights into the complex landscape of ADC design, particularly emphasizing the critical importance of target selection and mitigation of adverse effects.
The foundation of any successful ADC lies in its target antigen—proteins expressed on the surface of cancer cells that guide the conjugated antibody directly to malignant tissues. Ideally, these targets should be abundantly expressed on tumor cells and absent or minimally present on healthy tissues to avoid off-target toxicity. However, the identification of such ideal antigens remains a formidable hurdle. Most candidate targets display heterogeneous expression patterns within tumors and, crucially, are also present in normal tissues at varying levels, potentially triggering life-threatening side effects.
The development and clinical deployment of HER2-targeted ADCs illustrate this conundrum vividly. Trastuzumab deruxtecan, a notable third-generation ADC targeting HER2-positive cancers, has demonstrated remarkable efficacy in breast and gastric cancers. Yet, the underlying expression of HER2 in cardiac and pulmonary tissues poses a significant risk, with patients occasionally experiencing severe cardiotoxicity and respiratory diseases. This duality underscores how even effective ADCs can be compromised by the biology of their selected antigens, necessitating rigorous antigen distribution profiling beyond tumor sites.
Other targets, such as Trop2 and the epidermal growth factor receptor (EGFR), similarly betray the challenge of balancing efficacy and safety. Trop2, despite its therapeutic potential, has broad expression across normal epithelial tissues, resulting in widespread toxicity when targeted by ADCs. Likewise, EGFR-targeting conjugates, while potent, are prone to induce severe infusion reactions and ocular toxicities. These adverse outcomes reflect a narrow therapeutic window and highlight the urgent need for precision in antigen selection and ADC design.
Among emerging ADC targets, Claudin-18 (CLDN18) emerges as a beacon of promise. Unlike HER2, Trop2, or EGFR, Claudin-18 boasts restricted expression in normal tissues but is highly prevalent in several tumor types, particularly gastric cancers. Early-phase clinical trials utilizing CLDN18-directed ADCs report minimal adverse effects, positioning it as a safer alternative for targeted therapy. The success of Claudin-18-based ADCs may pave the way toward a new paradigm of high-efficacy, low-toxicity treatments, sparking renewed interest in exploring tissue-restricted antigens.
Critical to overcoming the inherent complexities of target selection is the integration of advanced technologies. Single-cell sequencing allows researchers to dissect intratumoral heterogeneity at an unprecedented resolution, revealing nuanced antigen expression patterns that could inform more selective targeting strategies. Simultaneously, artificial intelligence algorithms are being leveraged to predict antigen distribution and toxicity profiles, streamlining the identification of optimal target candidates and minimizing the risk of off-target effects.
Moreover, innovations in antibody engineering and linker chemistry remain indispensable for augmenting ADC efficacy and safety. The design of more stable linkers that release cytotoxic payloads exclusively within tumor cells, coupled with antibodies engineered for enhanced specificity, collectively shift the therapeutic window in favor of patient benefit. Such technological refinements ensure that ADCs can deliver their lethal cargo precisely where needed, sparing healthy tissues from collateral damage.
The pathway to broader ADC applicability also hinges on overcoming resistance mechanisms that tumors frequently develop. Cancer cells can alter antigen expression or enhance drug efflux systems, leading to therapy evasion. Strategies combining ADCs with immunotherapies or other chemotherapeutic agents hold immense promise in circumventing resistance, leveraging synergistic effects to enhance tumor cell killing and sustain clinical responses.
Despite these advancements, challenges remain formidable. The dynamic microenvironment of tumors, including hypoxia and immune modulation, influences antigen presentation and drug delivery efficacy. Additionally, interpatient variability adds layers of complexity to ADC administration, necessitating personalized treatment approaches and biomarkers to predict and monitor responses effectively.
The review poignantly characterizes the “Icarian flight” of ADCs—a metaphor illustrating the ambition and peril of these therapies as they soar toward transformative cancer treatment but risk downfall without cautious calibration. Our collective endeavor to harness ADCs safely and effectively demands multidisciplinary collaboration, spanning molecular biology, clinical oncology, bioinformatics, pharmacology, and beyond.
Looking forward, the fusion of cutting-edge science with clinical insight offers a compelling roadmap. Continued exploration of novel antigens such as Claudin-18, coupled with adaptive trial designs and real-time biomarker assessments, will refine therapeutic indices. Furthermore, deepening our understanding of tumor biology through spatial transcriptomics and advanced imaging will enable more precise ADC deployment.
In conclusion, antibody-drug conjugates embody a powerful but intricate weapon in the cancer therapy arsenal. The delicate interplay of antigen selection, payload potency, antibody specificity, and patient heterogeneity dictates their success or failure. Optimizing these variables through technological innovation and biological insight holds the key to expanding the impact of ADCs beyond current limitations, ultimately delivering safer and more effective treatments to patients worldwide.
Subject of Research: Not applicable
Article Title: The Icarian flight of antibody-drug conjugates: target selection amidst complexity and tackling adverse impacts
News Publication Date: 15-Jan-2025
Web References: 10.1093/procel/pwaf002
Image Credits: Han Liu, Hongye Zeng, Xiaojing Qin, Wenjing Ning, Lin Xu, Shiting Yang, Xue Liu, Wenxin Luo, Ningshao Xia