A groundbreaking new study analyzing pharmaceutical use across the United States has shed light on complex patterns of medication access and equity among diverse racial and ethnic groups. Drawing from a cross-sectional evaluation of 143 health conditions in all 50 states plus Washington, DC, the research reveals stark disparities in prescription medication fills that challenge prior assumptions and demand urgent public health attention. These findings underscore the necessity for nuanced, localized strategies to promote pharmacoequity, ensuring that all populations receive appropriate treatment supported by robust data.
The raw data illuminate an intriguing paradox: when measured on a per capita basis, white populations in the U.S. exhibit the highest pharmaceutical consumption rates. This elevated rate reflects, in part, systemic advantages related to healthcare access, insurance coverage, and socioeconomic factors that facilitate prescription fulfillment. In contrast, Asian or Pacific Islander and Hispanic populations consistently show lower per capita pharmaceutical use, suggesting potential barriers or underutilization. However, the story gains complexity when adjustments for age distribution and disease prevalence are incorporated.
Standardizing for these variables across 52 health conditions with available comparative data reveals a significantly different pattern. Notably, Black populations demonstrate substantially lower prescription fill rates compared to the national average for all groups combined. This adjustment accounts for disease burden and demographic differences, highlighting that the observed disparities are not simply due to variations in health needs but may represent systemic inequities in healthcare delivery or access.
The implications of these patterns are profound for public health policy and clinical practice. Lower prescription fills after adjustment suggest potential under-treatment or barriers to receiving necessary medications for Black Americans. These disparities may contribute to worsened health outcomes and perpetuate existing inequities in chronic disease management, morbidity, and overall quality of life. Identifying and addressing the root causes of these gaps is crucial to achieving equitable healthcare.
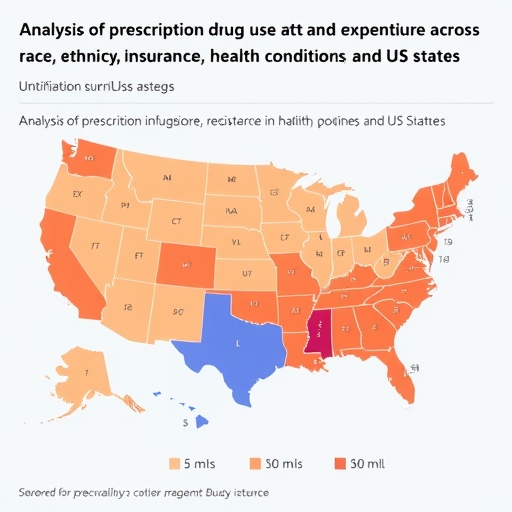
Moreover, the study details that these pharmaceutical use disparities are not uniform across the country but exhibit significant variation from state to state. Such geographic variability implies that localized social determinants, healthcare infrastructure, state policies, and cultural factors heavily influence medication access. This heterogeneity demands region-specific interventions and collaborative efforts between policymakers, healthcare providers, and community organizations.
The methodological rigor of the study stands out, given its scope and adjustments. By focusing on a comprehensive set of 143 health conditions, it provides a broad lens on pharmacotherapy usage across multiple disease domains rather than a narrow focus. The standardization for age and disease prevalence adds a layer of sophistication, allowing for fair comparisons across demographic groups and reducing confounding biases. The use of prescription fill data also offers a pragmatic window into actual medication adherence and access rather than mere prescribing behavior.
Pharmacoequity—the principle of equitable distribution and utilization of pharmaceutical interventions—is emerging as a critical concept in health equity research. This study contributes valuable empirical evidence highlighting persistent gaps in medication use that can exacerbate health disparities. Though access to healthcare coverage has improved over recent decades, this research underscores that disparities remain in actual medication uptake after treatment is prescribed, signaling systemic barriers beyond insurance alone.
Potential contributors to these disparities include socioeconomic status, healthcare literacy, provider biases, pharmacy deserts, and social determinants such as transportation or cultural mistrust. The study’s findings signal that policies must extend beyond insurance coverage expansions to address these multifaceted factors impacting medication accessibility and adherence. Targeted community outreach, patient education, culturally competent care, and improved pharmacy access could mitigate these barriers.
Furthermore, the research provokes reflection on the role of healthcare providers and systems in recognizing and rectifying inequities in pharmaceutical care. Clinical guidelines and quality metrics must incorporate equity considerations, encouraging clinicians to identify and support patients at risk of under-treatment. Health systems might employ real-time data analytics and population health management approaches to monitor prescription fills and adherence by race and ethnicity, enabling early intervention.
This study’s cross-sectional nature limits the ability to infer causality or track longitudinal trends; nonetheless, it establishes a crucial foundation for ongoing research. Future investigations might leverage longitudinal datasets to explore temporal changes in pharmacoequity and assess the impact of emerging policies or interventions. Additionally, disaggregating data within racial and ethnic subgroups could uncover nuanced disparities and unique needs, enriching the evidence base for tailored programs.
Given the intricate interplay between health conditions, demographic factors, and geographic context, the researchers emphasize that a one-size-fits-all approach to improving pharmacoequity is unlikely to succeed. Instead, localized, disease-specific, and culturally adaptive strategies are essential. These might include state-level policy reforms, targeted funding for underserved communities, and integration of pharmacists into multidisciplinary care teams focusing on equity.
The broader narrative emerging from this study aligns with recent calls from health equity advocates who stress that true health equality requires equitable access to medications—one of medicine’s most potent tools. Without equitable pharmaceutical use, the promise of modern medicine remains unfulfilled for many vulnerable populations, perpetuating avoidable suffering and health disparities.
In sum, this comprehensive analysis presents compelling evidence of racial and ethnic disparities in prescription fills across the U.S., adjusted for underlying health needs. It challenges healthcare stakeholders to redouble efforts in understanding, monitoring, and rectifying inequities in medication use at both national and local levels. By fostering pharmacoequity, the healthcare system can move closer to delivering on the promise of high-quality, accessible care for all Americans.
Subject of Research: Racial and ethnic disparities in prescription medication use across the United States adjusted for age and disease prevalence.
Article Title: Not available.
News Publication Date: Not available.
Web References: Not available.
References: (doi:10.1001/jamahealthforum.2025.2329)
Image Credits: Not available.
Keywords: Drug research, Drug costs, Racial differences, Ethnicity, Population, United States population, Data analysis, Age groups