Antenatal depression, a significant contributor to maternal morbidity, continues to pose a critical public health challenge worldwide, with profound implications for both mothers and their offspring. Despite its global prevalence, region-specific data—particularly from populous and diverse countries such as China—remain scarce and fragmented. Addressing this knowledge gap, a comprehensive, large-scale epidemiological study led by Professors Hefeng Huang and Yanting Wu from the Obstetrics and Gynecology Hospital at Fudan University has meticulously mapped the prevalence and correlates of antenatal depression across multiple regions of China. This cross-sectional investigation, encompassing over 100,000 pregnant women from 27 public hospitals spanning 11 provinces and metropolitan areas, provides unprecedented insight into the burden of depressive symptoms during pregnancy and their socioeconomic determinants.
Antenatal depression is characterized by clinically significant depressive symptoms during pregnancy, distinct in that it not only compromises maternal well-being but also poses detrimental effects on fetal development and postnatal adaptation. Left undiagnosed or untreated, it often extends into the postpartum period, exacerbating risks for adverse outcomes including preterm birth, low birth weight, and impaired mother-infant bonding. Thus, delineating its prevalence and risk factors is essential for informing culturally tailored interventions and health policy.
The study employed the Edinburgh Postnatal Depression Scale (EPDS), a validated screening tool, to quantify depressive symptoms during the third trimester of pregnancy. An EPDS score greater than nine was adopted as the threshold for probable antenatal depressive symptoms, whereas scores above twelve indicated probable clinical depression necessitating further management. By integrating sociodemographic, behavioral, and psychosocial variables, the research elucidated multifactorial influences shaping depression risk, spanning from basic demographics to nuanced relational dynamics such as partner support.
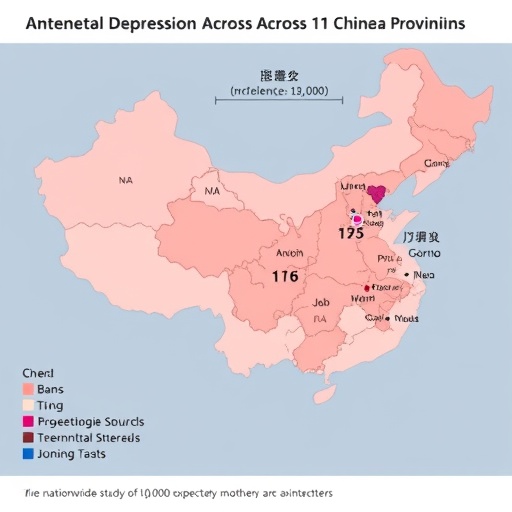
Regional disparities emerged as a significant theme. The northern provinces of Liaoning and Henan exhibited the highest prevalence rates, with approximately 30.8% of pregnant women screening positive for possible depression and 15.7% for probable depression. Contrastingly, eastern regions including Shanghai, Zhejiang, Jiangxi, and Anhui reported relatively lower rates, with 24.5% and 10.6% for possible and probable depression, respectively. These geographic differences may reflect variations in socioeconomic development, healthcare infrastructure, cultural attitudes towards mental health, and availability of social support networks.
Detailed statistical analyses underscored a constellation of factors significantly associated with antenatal depression. Young maternal age surfaced as a vulnerability factor, potentially linked to limited life experience and social resources. Low educational attainment and family income underscored the socioeconomic gradient of mental health, revealing how material deprivation exacerbates psychological distress during pregnancy. Additionally, unemployment, unmarried or divorced status, and solitary living arrangements compounded risk, highlighting the critical role that social isolation plays in mental well-being.
Pregnancy-specific factors were also implicated. Unintended pregnancies and multiple gestations were associated with higher depression scores, possibly due to increased physical demands and psychosocial stressors. Lifestyle behaviors, notably tobacco and alcohol use, further elevated depressive symptomatology, reflecting the bidirectional relationship between substance use and mood disorders. Poor sleep quality emerged as another salient correlate, consistent with the neurobiological interplay between sleep disruption and affective regulation.
Crucially, the study illuminated the protective influence of social support, with partner support identified as a key modifying factor. Adequate emotional and practical support from partners attenuated the impact of non-modifiable risk factors such as age, educational level, and employment status on depressive symptoms. This finding aligns with extant literature emphasizing the buffering role of interpersonal relationships in perinatal mental health and signals a promising target for intervention. Enhancing partner involvement and support mechanisms could thus represent a cost-effective strategy to mitigate the high burden of antenatal depression.
From a methodological standpoint, this investigation represents a landmark in scale and scope. The recruitment of 100,200 pregnant women across disparate geographical and socio-economic strata enhances the generalizability and robustness of findings. Use of validated psychometric tools and rigorous multivariate logistic regression analyses ensured precise estimation of associations while controlling for confounding variables. The cross-sectional design, albeit limiting causal inference, provides essential epidemiological benchmarks to guide subsequent longitudinal and interventional studies.
The implications of these findings extend beyond China’s borders, offering critical lessons for global maternal mental health initiatives. The high prevalence rates underscore that antenatal depression requires urgent integration into routine prenatal care, with systematic screening and referral pathways. Moreover, understanding contextual risk factors fosters precision public health approaches, wherein tailored psychosocial support and resource allocation can address distinct community needs.
Future research should endeavor to elucidate the biological and psychosocial mechanisms underpinning these associations, including exploration of hormonal, inflammatory, and neurocognitive pathways. Furthermore, longitudinal follow-up studies could clarify the trajectories of antenatal depression and its impact on postpartum outcomes, child development, and family dynamics. Importantly, implementation research is needed to evaluate the effectiveness of partner-focused interventions and community-based support programs in diverse cultural contexts.
In conclusion, this unprecedented large-scale multi-regional study furnishes compelling evidence that antenatal depression affects over one-quarter of pregnant women in China, with marked regional and sociodemographic disparities. The identification of modifiable risk factors, especially the critical protective role of partner support, provides actionable insights for healthcare providers and policymakers. Addressing antenatal depression with culturally sensitive, family-centered strategies will be vital in safeguarding maternal and neonatal health, ultimately contributing to the reduction of the global burden of perinatal mental illness.
Subject of Research: Prevalence, risk factors, and protective influences associated with antenatal depression among pregnant women in China.
Article Title: Prevalence and related factors of antenatal depression in 11 provinces and cities of China: a 100,000 population-based study.
Web References: http://dx.doi.org/10.1016/j.scib.2025.06.031
Image Credits: ©Science China Press
Keywords: Antenatal depression, perinatal mental health, Edinburgh Postnatal Depression Scale, partner support, socioeconomic factors, China, maternal morbidity, epidemiology, pregnancy, psychosocial risk factors.