In a striking revelation that challenges assumptions about public health progress, a recent comprehensive study led by researchers at Boston University School of Public Health (BUSPH) has uncovered that excess mortality in the United States persists at alarmingly high levels, even years after the acute phase of the COVID-19 pandemic. The research, published in JAMA Health Forum, delves deep into comparative mortality data spanning over four decades, revealing a distressing and sustained mortality disadvantage that renders over 1.5 million deaths in 2022 and 2023 as “missing Americans” — deaths that could arguably have been prevented if the U.S. mortality rates aligned with those of other high-income nations.
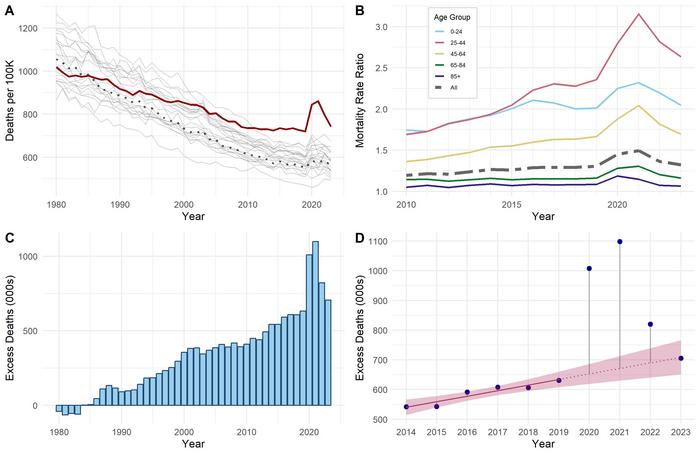
This analytical tour de force traces mortality trends from 1980 through 2023, employing meticulous age-standardization techniques to adjust for demographic differences and juxtaposing U.S. death rates against an average derived from 21 peer countries including Australia, Canada, France, Japan, and the United Kingdom. The findings emphasize that while the COVID-19 pandemic exacerbated existing mortality discrepancies, the roots of this public health crisis extend well before the viral onslaught, reflecting systemic and structural failures in healthcare access, social policy, and prevention strategies.
Excess deaths, defined as the number of deaths above what would be expected if U.S. mortality mirrored peer countries, peaked at nearly 1.1 million in 2021 during the height of the pandemic. However, the subsequent reduction to approximately 820,000 in 2022 and 705,000 in 2023 did not signify a true recovery but rather a reversion to a concerning upward trajectory that predates COVID-19. Crucially, the 2023 tally remains significantly higher than the pre-pandemic figure of 631,000 in 2019, illustrating that the pandemic’s shadow looms larger and longer than anticipated.
The disproportionate impact on working-age adults is particularly harrowing. Nearly half – 46% – of all deaths among Americans under 65 could potentially have been averted if U.S. age-specific mortality rates conformed to those of other wealthy nations. This persistent age-related vulnerability underscores a critical public health dilemma, highlighting how crises such as drug overdoses, gun violence, and cardiometabolic diseases systematically erode vitality within a segment of the population traditionally considered to be in their productive prime. The continuity of these disparities before, during, and after the pandemic signals deeply ingrained social determinants and health system inadequacies that disproportionately affect younger Americans.
The study’s lead author, Dr. Jacob Bor, an epidemiologist and associate professor at BUSPH, describes this phenomenon as a “protracted health crisis,” one that has quietly unfolded beyond public gaze while claiming millions of avoidable lives. The metaphor of “missing Americans” poignantly encapsulates the magnitude of this issue, reflecting a failure at the population level that transcends individual behavior and signals profound policy neglect.
By examining mortality data exceeding 107 million U.S. deaths and more than 230 million deaths from peer countries, the research team applied rigorous counterfactual modeling to estimate excess mortality. This approach accounted for varying age distributions and leveraged standardized mortality ratios, ensuring robust, comparable metrics. Their data shows that between 1980 and 2023, the U.S. endured approximately 14.7 million excess deaths relative to its peers — a staggering figure that points to persistent and systemic health disadvantages.
Importantly, the study highlights that COVID-19 acted as an accelerant rather than an originator of mortality disparities. The virus precipitated a sharp increase in excess deaths in 2020 and 2021 but did so against a backdrop of existing vulnerabilities, including overdose epidemics driven by narcotics and opioids, escalating gun violence, fatal car crashes, and preventable cardiometabolic conditions such as heart disease and diabetes. These chronic challenges underscore the complex etiology of ongoing excess mortality, implicating societal, policy, and healthcare system failures.
Senior author Dr. Andrew Stokes of BUSPH points to the broader structural weaknesses exposed by the pandemic. In many high-income countries, robust universal health coverage, comprehensive social safety nets, and coordinated public health initiatives mitigated the pandemic’s toll. In contrast, the U.S.’s fragmented healthcare system, marked by inequities in access and quality, alongside social determinants such as economic instability and political polarization, have stymied effective responses both to COVID-19 and to foundational causes of premature death.
The social and political landscape further complicates U.S. efforts to bridge the mortality gap. Public distrust of government institutions and increasing political divisiveness undermine consensus on implementing evidence-based health policies. These barriers hinder the adoption of proven practices seen in peer countries, such as harm reduction approaches for substance abuse, stricter gun regulation, and expanded preventive care.
Researchers emphasize the urgency of reversing these trends through informed policy interventions. Lessons from international counterparts suggest that investment in universal healthcare systems, strengthened social safety mechanisms, and comprehensive environmental and regulatory frameworks can promote healthier, longer lives and reduce preventable deaths. The failure to leverage these insights, coupled with austerity measures targeting health and social programs, threatens to widen disparities further.
Additionally, the research team warns that recent governmental policies, including cuts to public health funding, reductions in scientific research investment, and diminished data transparency, could exacerbate the mortality disadvantage. These policies risk perpetuating the cycle of preventable deaths by weakening the infrastructure necessary to identify, monitor, and address health crises effectively.
The study also aligns with a parallel investigation published earlier in 2025 revealing that drug-related deaths now constitute the leading cause of mortality among adults aged 25 to 44. This grim statistic emphasizes the entrenched nature of the overdose epidemic and the critical need for multisectoral public health interventions targeting addiction and mental health.
Moving forward, the researchers advocate for comprehensive, multi-level policy strategies that espouse equity, evidence, and prevention. Future investigations will seek to disentangle the specific causes driving these mortality differences, integrating epidemiological, sociological, and policy perspectives to chart actionable paths toward closing the mortality gap.
In closing, this sobering analysis reinforces that the U.S. faces a formidable public health challenge whose magnitude rivals historic crises. Addressing this simmering mortality epidemic requires concerted efforts to overhaul healthcare infrastructure, revive social safety nets, and embrace pragmatic, evidence-informed policies that prioritize population health. Without such transformation, the narrative of “missing Americans” will continue, chronicling the preventable loss of millions of lives and a national failure to safeguard the health of its people.
Subject of Research: People
Article Title: Excess Deaths Before, During, and After the COVID-19 Pandemic
News Publication Date: 23-May-2025
References:
Bor J, et al. Excess Deaths Before, During, and After the COVID-19 Pandemic. JAMA Health Forum. 2025; DOI: 10.1001/jamahealthforum.2025.1118.
Image Credits: Boston University School of Public Health
Keywords: Mortality rates, Viral infections, Public health, Epidemics, Substance abuse, Drug abuse, Violence, Gun violence, Cardiovascular disorders, Cardiovascular disease, Heart failure, Heart disease, Health care, Adults, Young people, Narcotics addiction, Opioid addiction, COVID 19, Long Covid