A groundbreaking study from Shinshu University illuminates the profound and lasting effects of postpartum maternal depression and early mother-to-infant bonding on children’s psychosocial development well into middle childhood. While the deleterious short-term consequences of postpartum depression on infant development have been studied extensively, this latest research advances our understanding by unraveling how the early quality of mother-infant bonding intermediates the trajectory of emotional and behavioral outcomes at the pivotal developmental stage of sixth grade.
Postpartum depression, characterized by pervasive feelings of sadness, anxiety, and emotional withdrawal following childbirth, afflicts approximately one in six mothers globally, with similar prevalence documented in Japan. This condition disrupts not only the mother’s mental health but also hampers the establishment of secure attachment between mother and infant. The integrity of early bonding experiences is critically influential in shaping a child’s socioemotional framework, affecting cognitive development, emotion regulation, and future interpersonal relationships.
The research team, spearheaded by Associate Professor Daimei Sasayama together with Professor Hideo Honda of Shinshu University’s Departments of Psychiatry and Child and Adolescent Developmental Psychiatry, employed a longitudinal design to probe the nuanced interplay between postpartum depression, bonding quality, and subsequent child psychosocial adjustment. Their extensive survey encompassed 245 mother–child dyads from Okaya, Japan, whose children were born between 2009 and 2012, providing a robust dataset to assess long-term developmental outcomes.
Maternal depressive symptoms were quantified using the Edinburgh Postnatal Depression Scale (EPDS), a standardized instrument validated globally for postpartum mood assessment. Mother-to-infant bonding was measured via the Japanese variant of the Mother-to-Infant Bonding Scale (MIBS-J), capturing affective and behavioral deficits related to the early attachment process. Child behavioral and emotional difficulties were evaluated through the Strengths and Difficulties Questionnaire (SDQ), with data converging from self-reports and caregiver observations when the children reached sixth grade.
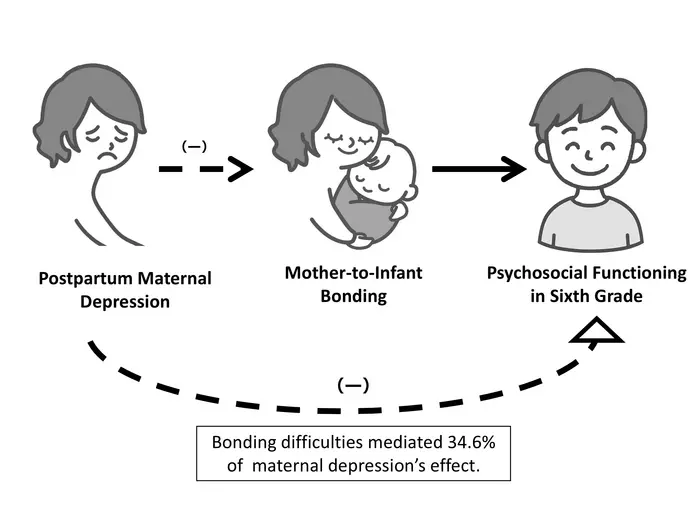
The findings revealed that 17.1% of participating mothers met criteria indicative of postpartum depressive symptomatology, paralleling national prevalence benchmarks. Critically, these symptoms exerted both direct effects on child difficulties and indirect effects mediated via impaired mother-to-infant bonding. Quantitatively, the study demonstrated that approximately 34.6% of the influence of maternal postpartum depression on child psychosocial challenges was transmitted through disruptions in early bonding, providing empirical validation to the mediation hypothesis.
Beyond confirming these associations, the research also uncovered sex differences in psychosocial outcomes, with male children exhibiting notably higher total difficulties, especially in conduct problems and hyperactivity-inattention domains. This sex-based disparity aligns with broader developmental psychopathology literature indicating heightened vulnerability among boys to behavioral issues following early adversities.
Technically, the study’s multidimensional approach integrates psychometric rigor with temporal depth, underscoring that early maternal mental health interventions should not only target depressive symptoms but prioritize the restoration and facilitation of healthy bonding practices. This interplay suggests a bidirectional causality where postpartum depression compromises bonding, which in turn exacerbates child difficulties, highlighting a critical window for preventive strategies.
From a mechanistic perspective, impaired bonding during the sensitive postpartum period may dysregulate neurobiological systems implicated in stress response and emotional regulation, such as the hypothalamic-pituitary-adrenal axis and oxytocinergic pathways. Such neurodevelopmental perturbations potentially lay the groundwork for behavioral dysregulation and internalizing problems observed years later in middle childhood.
Looking forward, Dr. Sasayama and colleagues advocate for the expansion of research to dissect which specific depressive symptoms wield the most detrimental effects on bonding quality, alongside incorporating genetic, socioeconomic, and environmental variables. Such holistic inquiry could refine targeted intervention designs, tailoring support to mothers displaying distinct depressive profiles and environmental contexts.
Moreover, the study accentuates societal implications, advocating for enhanced postpartum screening protocols and mother-infant bonding support within healthcare systems. Early psychosocial interventions that improve maternal affective states and attachment security can disrupt the transgenerational transmission of psychopathology and optimize developmental trajectories for children.
In sum, this pioneering research not only enriches scholarly discourse on maternal mental health’s enduring imprint on child development but also offers actionable insights for clinicians, policymakers, and families. By highlighting mother-to-infant bonding as a critical mediator, it charts a transformative path towards mitigating long-term child psychosocial difficulties through early detection and nurturing of maternal-infant relationships.
This study’s publication in the high-impact journal Archives of Women’s Mental Health on April 15, 2025, marks a significant milestone in perinatal psychiatry and developmental psychology. It prompts a paradigm shift emphasizing the integration of bonding-focused interventions in maternal health programs — a promise to revolutionize strategies aimed at fostering healthier futures in subsequent generations.
As the global community grapples with rising mental health burdens, understanding the intricate relational dynamics during infancy emerges as a vital frontier. This research not only reaffirms the essence of secure early attachments but also charts scientifically grounded pathways for intervention, underscoring the profound interconnectedness of maternal well-being and child development.
Subject of Research: People
Article Title: Postpartum maternal depression, mother-to-infant bonding, and their association with child difficulties in sixth grade
News Publication Date: 15-Apr-2025
Web References:
https://link.springer.com/article/10.1007/s00737-025-01585-y
References:
Sasayama, D., Honda, H., et al. (2025). Postpartum maternal depression, mother-to-infant bonding, and their association with child difficulties in sixth grade. Archives of Women’s Mental Health. DOI: 10.1007/s00737-025-01585-y
Image Credits:
Daimei Sasayama from Shinshu University, Japan
Keywords:
Mental health, Clinical psychology, Developmental psychology, Human relations, Mothers, Children