Miami, February 19, 2026—Recent research published in the January 2026 issue of Chronic Obstructive Pulmonary Diseases: Journal of the COPD Foundation presents compelling evidence that neighborhood-level socioeconomic factors significantly influence the incidence of emergency department visits and hospitalizations for chronic obstructive pulmonary disease (COPD) exacerbations. The study reveals that residents living in neighborhoods marked by higher poverty rates, greater levels of uninsured populations, and lower educational attainment face elevated risks of severe COPD flare-ups requiring acute medical care.
COPD, which encompasses emphysema and chronic bronchitis, is a progressive respiratory disease afflicting over 30 million people in the United States alone, and it ranks as the fourth leading cause of death globally. The pathophysiology of COPD involves airflow obstruction due to chronic inflammation, often triggered or worsened by genetic predispositions but predominantly caused by environmental factors such as tobacco smoke exposure and air pollution. These insults contribute to the irreversible destruction of lung tissue and airway remodeling, leading to chronic respiratory symptoms and functional impairment.
Acute exacerbations of COPD (AECOPD) represent episodes of abrupt symptom worsening, characterized by increased dyspnea, sputum production, and coughing. These episodes often precipitate urgent emergency department visits and hospital admissions, with substantial ramifications for patients’ health outcomes, healthcare utilization, and economic burden. Despite advances in COPD management, preventing exacerbations remains a critical challenge due to the complex interplay of individual vulnerability and contextual factors.
The investigative team conducted an observational ecological study utilizing robust patient-level data spanning five years (2016–2020) from census tracts within Travis County, Texas. Census tracts, as standardized geographic units averaging around 4,000 residents, provide a nuanced framework to correlate neighborhood attributes with health outcomes while minimizing variability in demographic and socioeconomic factors. By analyzing nearly 10,000 COPD-related emergency department visits, hospitalizations, and subsequent 30-day readmissions, the study sought to elucidate the spatial heterogeneity and social determinants influencing acute COPD care utilization.
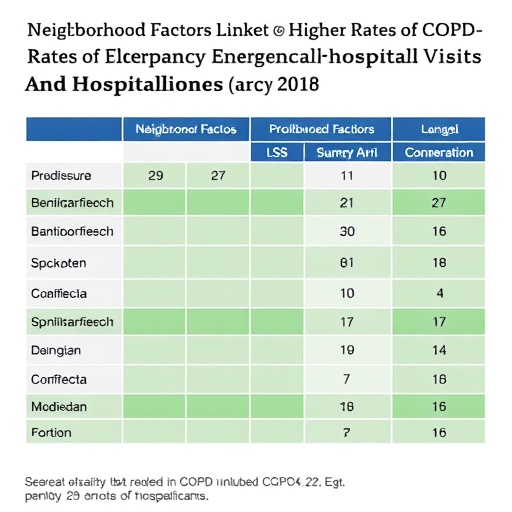
Geospatial analyses uncovered discernible clustering patterns in emergency visits and hospital admissions tied to neighborhoods characterized by socioeconomic deprivation. Factors such as household poverty rates, the proportion of uninsured individuals, and lower educational attainment emerged as significant correlates of increased acute care use. Intriguingly, hospital readmission rates within 30 days did not exhibit corresponding geographic clustering, suggesting that readmissions may be influenced more by clinical factors or healthcare system-level interventions rather than neighborhood environment.
The findings underscore the imperative to expand COPD intervention frameworks beyond individual clinical care to encompass population health strategies that address social determinants of health. Tailoring public health initiatives to mitigate poverty, improve insurance coverage, and elevate educational opportunities could attenuate the incidence of exacerbations requiring emergent care. This approach advocates for multisectoral collaborations involving healthcare providers, policymakers, and community organizations to implement targeted, neighborhood-specific preventive measures.
Dr. Trisha M. Parekh, D.O., MSPH, lead author and pulmonary specialist at Dell Medical School, University of Texas at Austin, emphasized the study’s translational value: “Recognizing the influence of socio-environmental contexts on COPD exacerbation risks can inform policies and resource allocation that seek to diminish healthcare disparities. This integration of individual risk profiles with neighborhood-level data enables precision public health approaches to enhance quality of life and reduce healthcare costs.”
Such population-based studies complement clinical research focused on physiological and genetic susceptibility to COPD exacerbations. They help create holistic models encompassing environmental exposures, health behaviors, healthcare access, and social vulnerability. Addressing these multifaceted determinants through comprehensive strategies promises substantial reductions in disease exacerbations and associated morbidity.
The study’s methodological rigor, leveraging a large sample size and precise geospatial analysis, lends credibility to its conclusions. However, the authors acknowledge limitations inherent in ecological studies, including potential unmeasured confounders and the inability to infer causality. Future longitudinal research incorporating individual-level data and environmental monitoring could further delineate mechanistic pathways linking neighborhood adversity to COPD exacerbation risk.
As COPD continues to impose a significant public health burden, integrating socio-economic context into surveillance and intervention frameworks represents a paradigm shift. Health systems could utilize geographic information systems (GIS) and community health assessments to proactively identify at-risk neighborhoods, deploying mobile health units, environmental remediation efforts, and enhanced outreach programs focused on smoking cessation, pollution reduction, and vaccination initiatives.
Ultimately, this research spotlights the critical role of socio-economic environments in respiratory health outcomes. By addressing neighborhood-level disparities, stakeholders can drive equitable improvements in COPD management, reduce preventable hospitalizations, and alleviate the profound individual and societal costs associated with severe COPD exacerbations.
Subject of Research: Neighborhood socioeconomic factors influencing COPD exacerbation-related acute care utilization
Article Title: Census Tract Variability in COPD Emergency Department, Hospitalization, and Readmission Rates in Travis County, Texas
News Publication Date: February 19, 2026
Web References: https://journal.copdfoundation.org/jcopdf/id/1553/Navigating-COPD-and-Bronchiectasis-A-COPD-Foundation-Survey-of-Differences-in-Patient-Perceived-Health-Care-Experiences-by-Sex
References: DOI 10.15326/jcopdf.2025.0663
Keywords: Chronic obstructive pulmonary disease, Emergency medicine, Socioeconomics, Health insurance, Poverty