In a groundbreaking study recently published in npj Viruses, researchers have unveiled a pivotal role for the STAT1 signaling pathway in regulating cholesterol metabolism within epithelial cells and its consequential impact on syncytia formation induced by respiratory syncytial virus (RSV). This revelation not only deepens our understanding of the intricate molecular interactions during viral infections but also opens new avenues for therapeutic intervention targeting host metabolism to control viral pathogenesis.
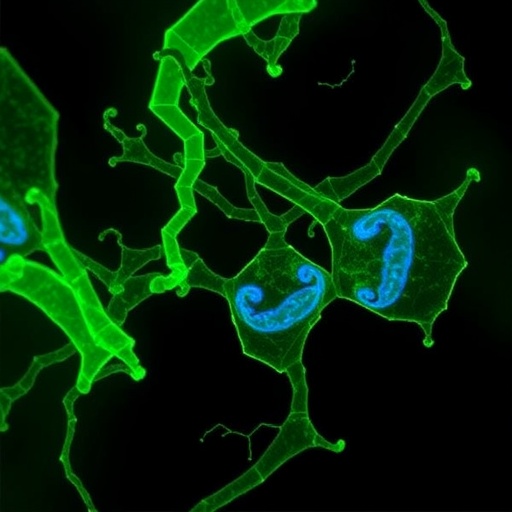
RSV remains a major pathogen, especially threatening infants and immunocompromised individuals, primarily through its ability to induce syncytia — multinucleated giant cells formed by the fusion of infected cells. Syncytia formation facilitates viral spread and exacerbates tissue damage, posing significant challenges to effective treatment. The molecular underpinnings that facilitate this process have remained elusive, but this recent study places the spotlight on how host cell cholesterol metabolism, governed by the STAT1 pathway, is central to this phenomenon.
Cholesterol, a fundamental component of the plasma membrane, is crucial for maintaining membrane fluidity and facilitating diverse cellular processes, including membrane fusion events. Pathogens like RSV exploit these cellular mechanisms, subverting host metabolic pathways to create an optimal environment for viral spread. The authors demonstrate that STAT1, a well-characterized transcription factor involved in immune responses, exerts precise control over cholesterol biosynthesis and homeostasis within epithelial cells, thereby influencing the biophysical properties of the cell membrane.
By employing a combination of genetic knockdown approaches and pharmacological modulation of STAT1 activity, the researchers effectively showed a marked alteration in cholesterol levels within epithelial membranes. This modulation led directly to either the amplification or suppression of syncytia formation when cells were exposed to RSV. Specifically, increased STAT1 activity corresponded with reduced cholesterol synthesis, resulting in decreased membrane fusogenicity and a lower incidence of syncytia, whereas inhibition of STAT1 had the opposite effect, promoting viral-induced cell fusion.
The study’s experimental design integrated cutting-edge lipidomics, single-cell RNA sequencing, and high-resolution imaging modalities to dissect the dynamic interplay between viral infection and host metabolic responses. Time-course analyses revealed that RSV infection triggers an early suppression of STAT1 signaling, a strategic viral evasion tactic to upregulate cholesterol biosynthesis and enhance membrane fusion susceptibility. This feedback loop between viral manipulation and host defense underscores the complexity of virus-host interactions and highlights the adaptability of RSV in exploiting host cell machinery.
Furthermore, the authors identify key downstream effectors of STAT1 signaling involved in the mevalonate pathway, a critical metabolic route for cholesterol generation. Notably, enzymes such as HMG-CoA reductase demonstrated altered expression patterns concomitant with STAT1 activity modulation, establishing a direct link between immune signaling pathways and metabolic control. Therapeutic agents targeting these metabolic enzymes, some of which are already in clinical use for cholesterol management in cardiovascular diseases, emerge as plausible candidates for repurposing to limit RSV pathogenesis.
Beyond the mechanistic insights, this study emphasizes the broader concept of metabolic regulation as an intrinsic component of antiviral immunity. STAT1, traditionally recognized for its role in mediating interferon responses and upregulating antiviral genes, now also emerges as a master regulator of lipid metabolism, integrating immune and metabolic pathways to shape infection outcomes. Such dual functionality may be crucial in other viral infections where membrane fusion and lipid composition play critical roles, suggesting that manipulating metabolic pathways could represent a universal antiviral strategy.
The implications for clinical management of RSV are profound. Current antiviral therapies primarily target viral proteins; however, these approaches often face challenges due to viral evolution and resistance. Targeting host factors such as STAT1 not only circumvents resistance but also offers the advantage of modulating a host pathway that impacts multiple downstream virus-supportive processes. Nonetheless, therapeutic modulation of STAT1 must be balanced carefully, given its vital role in orchestrating innate and adaptive immunity.
Intriguingly, this research advances the understanding of epithelial cell biology in the context of infection. Epithelial surfaces serve as the first line of defense and act as critical barriers to viral invasion. By elucidating how epithelial cholesterol metabolism is influenced by STAT1 and, in turn, governs viral-induced cell fusion, the study highlights the importance of cellular metabolic states in determining susceptibility to infection and disease severity.
The elaborate molecular choreography revealed here also offers a conceptual framework for future investigations into other respiratory viruses that induce syncytia, such as measles and human metapneumovirus. It raises the question of whether STAT1-mediated cholesterol regulation is a common host defense mechanism or if viruses have evolved distinct strategies to manipulate host lipid metabolism to their benefit.
In addition to biological insights, this study underscores the potential of integrating systems biology approaches with virology to unravel complex host-pathogen dynamics. Leveraging lipidomics alongside transcriptomic and proteomic data enriched the multi-dimensional understanding of the interplay between immune signaling and metabolism during viral infection, paving the way for the development of novel biomarkers and targeted therapies.
One particularly novel aspect of this research is the identification of STAT1 as a metabolic switch that toggles cholesterol synthesis pathways to either hinder or promote viral pathogen strategies like syncytia formation. This challenges the prevailing paradigm of STAT1 solely as an antiviral gene regulator and propels it into the realm of metabolic control, inviting a reevaluation of signaling pathways in the context of infection beyond canonical immune functions.
The translational potential of these findings is compelling. Repurposing cholesterol-lowering agents such as statins or exploring new molecules that modulate STAT1 activity could yield innovative antiviral therapies. Clinical trials assessing the efficacy of such interventions might not only attenuate RSV morbidity but could also contribute broadly to therapeutic strategies against a spectrum of enveloped viruses reliant on membrane fusion processes.
Finally, this study accentuates the importance of interdisciplinary research bridging immunology, virology, and metabolism. Understanding viruses through the lens of host metabolic regulation enriches the scientific narrative, offering profound insights into infection biology that have remained understudied until now. As such, the work of Agac, Ludlow, Knittler, and colleagues offers a transformative perspective that could redefine antiviral research paradigms in the coming decade.
Subject of Research: The study investigates how STAT1 signaling regulates cholesterol metabolism in epithelial cells and its impact on respiratory syncytial virus (RSV)-induced syncytia formation.
Article Title: STAT1 signaling controls cholesterol metabolism in epithelial cells and RSV-induced syncytia formation.
Article References:
Agac, A., Ludlow, M., Knittler, M.C. et al. STAT1 signaling controls cholesterol metabolism in epithelial cells and RSV-induced syncytia formation. npj Viruses 4, 10 (2026). https://doi.org/10.1038/s44298-026-00173-w
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s44298-026-00173-w