In a landmark study poised to redefine our understanding of Parkinson’s disease progression, researchers have discovered that a specific mutation in the LRRK2 gene, known as R1627P, significantly intensifies gut inflammation and the accumulation of α-synuclein aggregates—two pathological hallmarks increasingly recognized in the early stages of the disease. By utilizing rat models, the study intricately dissects the interplay between genetic predisposition and environmental factors, revealing a complex biological cascade that could revolutionize approaches to diagnosis and treatment.
Parkinson’s disease (PD) has long been characterized by the degeneration of dopaminergic neurons in the brain’s substantia nigra, primarily manifesting with motor symptoms such as tremors, rigidity, and bradykinesia. However, emerging evidence hints that the pathology of PD extends beyond the central nervous system, heavily implicating the gut and its extensive nervous network. In this groundbreaking investigation, the R1627P mutation of the leucine-rich repeat kinase 2 (LRRK2) gene emerges as a potent amplifier of environmental stress-induced chronic inflammation in the gastrointestinal tract, shedding light on novel peripheral mechanisms of disease initiation.
The LRRK2 gene is one of the most studied genetic loci implicated in familial and sporadic PD. Its protein product is a kinase involved in numerous cellular functions, including vesicular trafficking, mitochondrial homeostasis, and inflammatory responses. The R1627P mutation sits within an enzymatically critical domain, altering LRRK2 function in a way that exacerbates cellular stress responses when combined with environmental insults. This interaction appears to create a vicious cycle of sustained gut inflammation and neuronal compromise within the enteric nervous system.
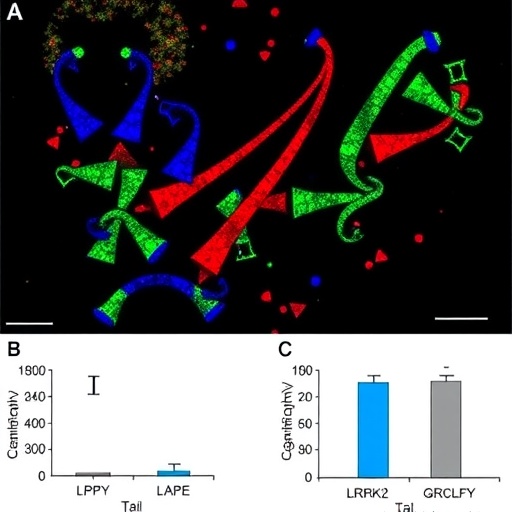
The research team employed rats genetically engineered to carry the LRRK2 R1627P mutation, exposing these animals to environmental factors known to induce inflammation, such as bacterial endotoxins and dietary toxins. Their findings demonstrated a pronounced increase in gut-derived chronic inflammatory markers compared to controls, along with a striking elevation in pathological α-synuclein accumulation. α-Synuclein, a presynaptic neuronal protein prone to misfolding and aggregation, forms the core of Lewy bodies—intracellular inclusions traditionally seen in brains of PD patients. Importantly, the study pinpoints the gut as an early site of α-synucleinopathy triggered or exacerbated by genetic and environmental interactions.
These insights critically support the Braak hypothesis, which suggests that PD pathology may ascend from the enteric nervous system to the brain via the vagus nerve. Detecting elevated α-synuclein aggregates in the gut of these mutant rats reinforces the notion that the gut acts not only as a reservoir but potentially as an origin point for the neurodegenerative cascade. This gut-brain axis connection is pivotal for reimagining early-stage biomarkers and preventative strategies targeting the gastrointestinal tract.
Chronic inflammation has emerged as a key pathogenic event in PD, but the mechanisms governing its initiation and perpetuation remain obscure. This study elucidates how the LRRK2 R1627P mutation primes intestinal immune cells to heightened reactivity upon exposure to environmental stimuli. This heightened immune sensitivity sustains a pathological inflammatory milieu, disrupting gut barrier integrity and facilitating the propagation of α-synuclein aggregates along enteric neurons. These processes collectively create a fertile ground for progressive neurodegeneration.
Moreover, by comparing wild-type rats to those carrying the R1627P mutation, the researchers found a clear gene-environment synergy that intensifies disease manifestation. Environmental insults alone induced moderate inflammation and protein aggregation, whereas the mutation dramatically amplified these phenotypes, underscoring the importance of genetic susceptibility in modulating disease risk. This nuanced understanding deepens the challenge of unraveling idiopathic PD cases that may involve subtle or unknown genetic variants influencing environmental response.
At the cellular and molecular levels, the study explored alterations in key signaling pathways. The mutated LRRK2 enhanced kinase activity resulted in aberrant phosphorylation of Rab GTPases, molecules crucial for vesicle trafficking and α-synuclein clearance. This dysregulation led to impaired autophagic flux and proteostasis within enteric neurons and immune cells, favoring the accumulation of toxic aggregates. These intimate molecular derangements provide actionable targets for therapeutic intervention to halt or reverse the pathological progression.
Beyond autophagy and inflammation, mitochondrial dysfunction was also markedly amplified in the R1627P mutant gut tissue. Mitochondria, vital for cellular energy and reactive oxygen species regulation, showcased decreased function and morphological disruptions in affected rats. This deficit contributes to increased oxidative stress, fueling a self-perpetuating cycle of cellular damage, α-synuclein misfolding, and immune activation. The comprehensive approach of this study sets a new benchmark for multifactorial analyses in neurodegenerative research.
Critically, the study’s focus on the gut environment opens promising avenues for diagnostic and therapeutic innovation. Gut biopsies may provide minimally invasive means to detect early α-synuclein deposits or inflammatory biomarkers in at-risk individuals. Meanwhile, pharmacological agents designed to modulate LRRK2 kinase activity or reinforce gut barrier integrity hold immense potential for disease modification. The dual targeting of genetic and environmental contributors offers a more effective model for personalized medicine in Parkinson’s disease.
The translational significance of these findings cannot be overstated. By highlighting that the LRRK2 R1627P mutation amplifies environmental risk factors, the research encourages a holistic view of Parkinson’s etiology that integrates lifestyle, microbial exposures, and genetic profiling. This paradigm shift could redefine clinical management, prompting earlier intervention strategies that precede overt motor symptoms, effectively pushing the frontier of neuroprotection.
Moreover, the model developed in this study represents a powerful platform for testing novel therapeutics. Scientists can now investigate potential treatments in a system that recapitulates the early and multifaceted pathology of PD, bridging the gap between experimental models and human disease. This advancement promises to expedite the arrival of efficacious, disease-modifying drugs.
The role of the gut microbiome, while not detailed explicitly in this study, naturally intertwines with chronic inflammatory states and α-synuclein propagation. Future extensions of this research may elucidate how microbial populations interact with susceptible host genetics like the LRRK2 R1627P mutation to modulate disease course. Unraveling this triad of genetics, environment, and microbiota will be crucial for a comprehensive framework of Parkinson’s pathogenesis.
In summary, this study marks a paradigm shift in Parkinson’s research by identifying the LRRK2 R1627P mutation as a critical amplifier of environmental toxin-induced chronic inflammation and α-synuclein aggregation in the gut. Such findings underscore the importance of examining peripheral origins of neurodegenerative diseases and fortify the concept of the gut-brain axis as a therapeutic battleground. As the scientific community advances toward integrated, multi-system models of Parkinson’s, this research stands as a beacon for future investigative and clinical endeavors.
As we deepen our understanding of how genetic mutations synergize with environmental insults to foster neuroinflammation and proteinopathy, the promise of early detection and intervention inches closer to reality. Ultimately, efforts inspired by these findings could transform the clinical landscape of Parkinson’s disease from reactive symptom management to proactive prevention and cure.
Subject of Research: The study investigates the influence of the LRRK2 R1627P mutation on environmental risk factor-induced chronic gut inflammation and α-synuclein aggregation in rat models, providing insight into Parkinson’s disease pathogenesis.
Article Title: LRRK2R1627P mutation amplifies environmental risk factors induced chronic inflammation and α-synuclein aggregation in the gut of rats.
Article References:
Pang, S., Lu, J., Wang, Y. et al. LRRK2R1627P mutation amplifies environmental risk factors induced chronic inflammation and α-synuclein aggregation in the gut of rats. npj Parkinsons Dis. (2026). https://doi.org/10.1038/s41531-026-01281-3
Image Credits: AI Generated