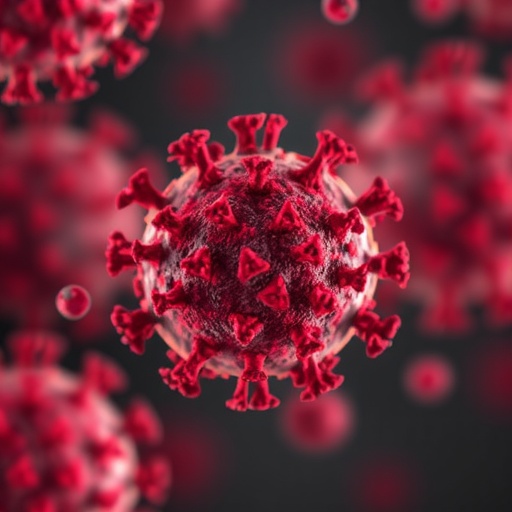
As we navigate through the lingering effects of the COVID-19 pandemic, one of the most alarming outcomes is the increasing prevalence of diabetes among those who have been infected with the virus. This condition, often referred to as post-COVID-19 diabetes, has emerged as a significant public health concern. Researchers have begun to peel back the layers of this phenomenon to understand the underlying mechanisms and potential risk factors. The findings indicate that COVID-19 may act as a catalyst for the development of diabetes, introducing a silent epidemic that has largely gone underreported amid the ongoing health crisis.
At the core of this discussion is the pathophysiology associated with COVID-19 infection. The SARS-CoV-2 virus, which causes COVID-19, has been shown to affect various organs, including the pancreas. This has led researchers to propose that the virus can lead to pancreatic injury and dysfunction, which are key contributors to the development of diabetes. Insights into how the viral particles interact with pancreatic cells provide a clearer understanding of the potential for COVID-19 to disrupt normal insulin production and glucose metabolism.
In addition to direct pancreatic implications, the inflammatory response triggered by COVID-19 cannot be overlooked. The body’s immune response to the infection can result in a cytokine storm, characterized by excessive inflammation that may also influence insulin sensitivity. Prolonged inflammation is known to play a role in insulin resistance, making individuals more susceptible to type 2 diabetes. The interplay between viral infection, inflammation, and metabolic health elucidates the complex web of factors that may lead to an increased diabetes risk.
Epidemiological studies have begun to show a concerning trend: individuals with a history of COVID-19 infection are at an elevated risk for developing diabetes, often within months of recovery. This delay in symptom manifestation poses a challenge for healthcare professionals, as patients may not associate their new diabetes diagnosis with their previous COVID-19 infection. Consequently, long-term health monitoring is crucial for patient populations regarded as high-risk due to COVID-19.
It is important to consider the demographic variables that play a role in post-COVID-19 diabetes. Several studies indicate that older adults, those with pre-existing health conditions, and individuals from certain ethnic backgrounds demonstrate a higher prevalence of diabetes following COVID-19. Identifying these at-risk groups can aid in developing targeted interventions and preventive measures. Public health initiatives must adapt to this new reality, recognizing diabetes as a potential sequela of COVID-19.
The current understanding of post-COVID-19 diabetes is still evolving, but crystal-clear connections are emerging. Viral load appears to correlate with the likelihood of developing diabetes. Patients with more severe COVID-19 cases, characterized by prolonged hospitalization and higher acuity, are increasingly showing signs of metabolic dysfunction. Moreover, emerging evidence suggests that even individuals with mild cases may experience metabolic disturbances that predispose them to diabetes.
At the forefront of this research is the urgent need for predictive models that can identify individuals at risk for post-COVID-19 diabetes. Advanced analytics, machine learning, and artificial intelligence (AI) methodologies are being harnessed to create these predictive tools. By integrating clinical data, demographic information, and markers of metabolic health, these models can potentially signal high-risk patients, prompting early intervention strategies.
Moreover, the treatment landscape for post-COVID-19 diabetes needs careful consideration. Unlike traditional diabetes paradigms, the intricacies of COVID-19-related diabetes necessitate a nuanced approach. Physicians may need to rethink management strategies, taking into account the unique pathophysiological ramifications of prior viral infection. The timeline for onset and management protocols will also require adjustments, ensuring that patients receive the appropriate care as soon as they present with symptoms.
Education and awareness campaigns are vital in addressing the growing concern of post-COVID-19 diabetes. Healthcare providers, patients, and the population at large must be made aware of the potential risks associated with COVID-19, emphasizing the importance of regular health checkups post-recovery. Understanding the signs and symptoms associated with diabetes can empower individuals to seek timely medical advice, potentially mitigating the impacts of this emerging epidemic.
As the global community continues to grapple with COVID-19, the implications stretch far beyond the immediate respiratory effects of the virus. Public health organizations can play a pivotal role in addressing the silent epidemic of post-COVID-19 diabetes by advocating for research funding and fostering collaborations among scientists, clinicians, and policymakers. Through concerted efforts, it may be possible to limit the long-term consequences of COVID-19 on metabolic health.
The story of post-COVID-19 diabetes is one interwoven with innovation and caution. While significant strides have been made in understanding this condition, the path forward will require dedication to ongoing research and patient advocacy. Stakeholders must prioritize this issue to cultivate a comprehensive understanding of how viral infection shapes long-term health outcomes.
As this field of research develops, it becomes increasingly critical for longitudinal studies to substantiate the emerging theories and secondary health effects associated with COVID-19. Each individual recovery story adds a valuable piece to the intricate puzzle of post-COVID-19 health challenges. Through collaborations, evidence-based practices, and patient engagement, the medical community can unearth preventive strategies and therapeutic interventions, ultimately aiming to reverse the trends of this silent epidemic.
Attention to post-COVID-19 diabetes represents an essential chapter in the ongoing narrative of the pandemic. By shedding light on this urgent health crisis, we can make strides toward a future where the impacts of COVID-19 extend only as far as the acute illness itself, rather than manifesting in chronic, debilitating conditions. As we stand on the threshold of new discoveries, it is clear that comprehensive care and education are paramount in addressing this looming public health challenge.
Subject of Research: Post-COVID-19 diabetes and its pathophysiology
Article Title: The Silent Epidemic Within the Pandemic: Pathophysiology and Prediction of Post-COVID-19 Diabetes
Article References:
Fang, H., Wang, Q. The silent epidemic within the pandemic: pathophysiology and prediction of post-COVID-19 diabetes.
J Transl Med (2026). https://doi.org/10.1186/s12967-026-07717-x
Image Credits: AI Generated
DOI:
Keywords: Post-COVID-19 diabetes, SARS-CoV-2, pathophysiology, insulin resistance, metabolic health, inflammation, epidemiology, predictive modeling, treatment strategies, public health.