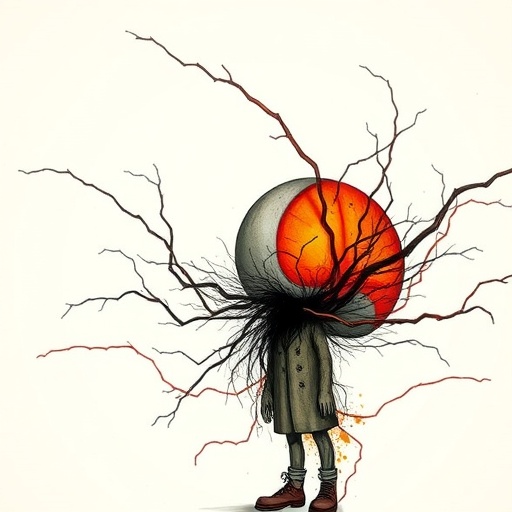
In a groundbreaking exploration of the intricate relationship between language, mental health, and the profound impact of mortality, Dr. C. Schorr’s latest research promises to illuminate a critical dimension of psychiatric education. With a title as evocative as “The Weight of Words: Learning Psychiatry at the Edge of Mortality,” this work is poised to challenge prevailing notions within the psychiatric community about how language shapes patient experiences and influences outcomes in mental health care.
At a time when the understanding of mental disorders is increasingly complex, Schorr’s research takes center stage, emphasizing the significance of verbal communication in psychiatric contexts. While textbooks focus on clinical symptoms and therapeutic techniques, this study argues that the words healthcare professionals choose can profoundly affect the therapeutic alliance, patient sensitivity, and outcomes. This insight extends beyond an academic exercise; it has real-world implications for practitioners who navigate the delicate interplay between language and patient care.
The concept of “the weight of words” draws attention to how specific terminologies used in psychiatric settings can evoke various emotional responses. Schorr’s research cites instances where the use of jargon or overly clinical language often alienates patients, creating barriers that hinder their ability to engage meaningfully in treatment. Conversely, when psychiatrists incorporate empathetic, relatable language, it fosters an environment where patients feel heard and understood, thus improving therapeutic rapport and enhancing treatment efficacy.
One of the most stirring elements of Schorr’s work is the acknowledgment of mortality’s grip on psychiatry. By situating the discourse within the framework of life and death, the importance of word choice becomes even more profound. When discussing terminal illness, depression, or severe mental health crises, the choice of words can drastically alter a patient’s psychological state. In this sense, psychiatric professionals carry not only the responsibility of diagnosis and intervention but also the ethical weight of how they communicate these realities to their patients.
While the influence of language within psychiatric care is not a new concept, Schorr’s research integrates empirical findings that reinforce the urgency of this topic. By compiling case studies and patient testimonials, Schorr showcases the repetitive patterns emerging from clinician-patient dialogues. The outcomes outlined in the study illustrate the stark contrasts between patients who received compassionate communication and those met with procedural or detached language.
Furthermore, Dr. Schorr addresses a critical gap in psychiatric training programs—namely, the neglect of communication skills in favor of technical knowledge. In a field that thrives on human interaction, the imperative to equip future psychiatrists with robust communication techniques is glaringly evident. Schorr argues for a paradigm shift in medical education, where language and empathy become integral parts of the psychiatric curriculum, thus preparing students for the emotional complexities they will encounter in practice.
The study also raises questions about the broader societal perceptions of mental health and wellness. Language plays a vital role in shaping public attitudes toward mental disorders, often grounding stigmas in derogatory or uninformed terminology. By advocating for mindful language use within not only clinical settings but also within media portrayals, Schorr’s work aspires to elevate the discourse around mental health. This commitment to changing the narrative is essential for fostering an informed and empathetic society at large.
Moreover, Schorr emphasizes the importance of ongoing dialogue among mental health professionals regarding the ethical implications of language. With mental health treatment increasingly under scrutiny—partly due to rising awareness of its vital importance—the pressure on psychiatrists to communicate effectively and sensitively cannot be overstated. The study proposes that engaging in reflective practices regarding word choice contributes to better self-awareness among clinicians and directly enhances patient care.
An innovative aspect of the research is the exploration of how digital communication—telehealth and online therapy mediums—impacts the language used by mental health professionals. The rapid transition to virtual platforms due to external circumstances, such as a global pandemic, has brought about novel challenges in maintaining compassionate communication through screens. Schorr advocates for the adaptation of empathetic language skills to fit this new medium, suggesting that the foundational principles of communication should persist regardless of the platform.
In addition to advocating for reform in communication practices, Dr. Schorr’s research is a call to action for mental health organizations and policymakers. By highlighting the necessity of training programs in language skills and empathetic communication, the study underscores a systemic issue that spans beyond individual practitioners to encompass entire healthcare frameworks. Investing in training that promotes verbal relational skills can yield meaningful advancements in patient-centered psychiatric care.
The ramifications of Schorr’s findings extend into therapeutic modalities that utilize language as the primary vehicle for healing—such as Cognitive Behavioral Therapy (CBT) and narrative therapy. By integrating insights from the weight of words, therapists can refine their techniques, enhancing their effectiveness and ensuring that patients feel a collaborative spirit in their healing journey. The transformative potential embedded within effective word choices cannot be overlooked in the therapeutic paradigm.
Central to the discourse outlined in this study is the quest to humanize psychiatric care. As mental health professionals increasingly navigate the complexities wrought by psychiatric disorders, the integration of linguistic consciousness can ground their practice in humanity. The power of compassionate words can lead to profound shifts in patient cognition and emotional states, challenging the stigma surrounding mental illness and paving the way for a new era of empathetic psychiatric care.
Finally, Schorr offers a hopeful vision for the future of mental health, one where the weight of words is recognized as a deciding factor in psychiatric success. By conscientiously choosing language steeped in empathy and understanding, mental health professionals have the potential to catalyze significant change, not just in individual lives but throughout the fabric of mental health care itself. This evolving dialogue around the intersection of language and psychiatry stands to benefit both practitioners and patients alike, bridging the gap between clinical acumen and human connection.
Subject of Research: The role of language and communication in psychiatric education and patient care.
Article Title: The Weight of Words: Learning Psychiatry at the Edge of Mortality
Article References:
Schorr, C. The Weight of Words: Learning Psychiatry at the Edge of Mortality.
Acad Psychiatry (2025). https://doi.org/10.1007/s40596-025-02295-4
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s40596-025-02295-4
Keywords: Language, Psychiatry, Communication, Patient Care, Empathy, Mental Health.