In a pioneering breakthrough that promises a paradigm shift in the treatment of diabetic retinopathy, researchers have unveiled a novel immunotherapy strategy targeting ceramide imbalance—a fundamental biochemical disruption implicated in the progression of this debilitating eye disease. The study, recently published in Cell Death Discovery, elucidates how the modulation of ceramide levels via targeted anti-ceramide immunotherapy can effectively reverse the pathological changes underlying diabetic retinopathy, offering new hope to millions affected worldwide.
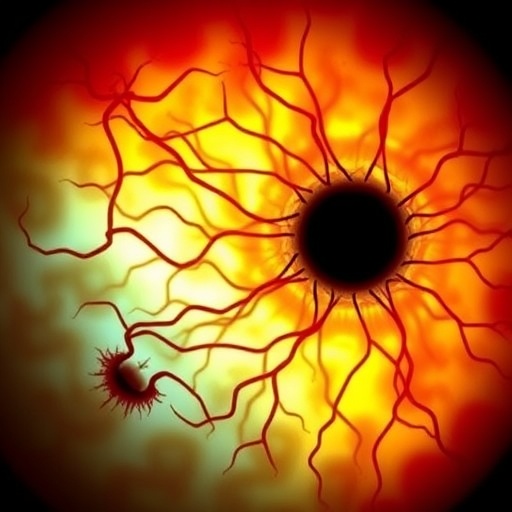
Diabetic retinopathy is a leading cause of blindness among working-age adults globally, characterized by progressive damage to the retinal blood vessels caused by chronic hyperglycemia. The intricate pathophysiology of this disease involves multifaceted molecular pathways, with lipid metabolism alterations emerging as crucial contributors. Among these, ceramide—a bioactive sphingolipid—has garnered attention for its role in mediating cellular stress, apoptosis, and inflammation within retinal tissues. However, until now, therapeutic interventions directly addressing ceramide imbalance have remained elusive.
The researchers spearheaded by Zhou, Li, Fu, and colleagues combined advanced lipidomics, immunological assays, and in vivo diabetic models to unravel how ceramide levels within retinal cells influence disease progression. Their findings reveal that diabetic conditions precipitate an aberrant accumulation of specific ceramide species, which in turn trigger endothelial dysfunction, increased vascular permeability, and retinal neuronal death. This cascade exacerbates microvascular damage, culminating in the hallmark features of diabetic retinopathy such as microaneurysms, hemorrhages, and neovascularization.
Recognizing ceramide’s pivotal role, the team developed an innovative anti-ceramide immunotherapy designed to selectively neutralize pathogenic ceramide molecules. Unlike conventional treatments, which primarily focus on managing hyperglycemia or inhibiting vascular endothelial growth factor (VEGF), this approach targets the biochemical root cause at the sphingolipid level. The immunotherapy employs monoclonal antibodies engineered to bind ceramide isoforms implicated in retinal damage, facilitating their clearance and restoring lipid equilibrium.
Preclinical trials demonstrated remarkable efficacy: treated diabetic animal models showed a significant reduction in retinal inflammation, vascular leakage, and neuronal apoptosis compared to controls. Optical coherence tomography and fluorescein angiography assessments corroborated these improvements, revealing preservation of retinal architecture and function. Intriguingly, the therapy’s benefits extended beyond halting progression, with evidence of partial reversal of established retinal lesions, a feat rarely achieved by existing modalities.
At the molecular level, administration of anti-ceramide antibodies modulated downstream signaling pathways associated with oxidative stress and cell death. The study highlights normalization of the ceramide-mediated activation of pro-apoptotic factors such as caspases, alongside attenuation of inflammatory cytokine release. This dual action underscores the therapeutic potential of immunomodulation in addressing both neurodegenerative and vascular components of diabetic retinopathy.
Moreover, the authors emphasize the therapy’s targeted specificity, which minimized systemic side effects and preserved physiological ceramide functions vital for cellular homeostasis. This precision reduces concerns surrounding off-target immune reactions, a common limitation in immunotherapies, suggesting a favorable safety profile for future clinical translation.
In addition to therapeutic implications, the research sheds light on ceramide’s function as a biomarker for disease severity and progression. Quantification of ceramide isoforms in ocular fluids could serve as a diagnostic tool or a measure of treatment response, facilitating personalized medicine approaches in diabetic retinopathy management.
The study’s innovative methodology integrates cutting-edge technologies, including mass spectrometry-based lipid profiling and genetic engineering for antibody optimization. This multidisciplinary approach exemplifies the future of translational research, bridging molecular insights with clinical applications to address previously intractable conditions.
Importantly, this work challenges the prevailing paradigm that diabetic retinopathy is an inexorably progressive disease, demonstrating that targeted molecular interventions can not only prevent but also potentially reverse retinal damage. This revelation opens avenues for earlier interventions, improved visual outcomes, and enhanced quality of life for patients.
While the promising findings warrant cautious optimism, the authors acknowledge the necessity for comprehensive clinical trials to evaluate long-term efficacy, optimal dosing regimens, and safety in diverse patient populations. The complexity of human diabetic retinopathy necessitates rigorous validation before widespread adoption.
The study also catalyzes interest in exploring ceramide-targeting immunotherapies for other sphingolipid-related disorders beyond ophthalmology, including neurodegenerative diseases and metabolic syndromes, underscoring the broad therapeutic potential of this strategy.
Collaborations among clinicians, immunologists, and pharmacologists will be critical to translate these insights into viable treatments. Concurrently, pharmaceutical development efforts must address formulation stability, delivery mechanisms, and immunogenicity to ensure patient accessibility and adherence.
In conclusion, this landmark research heralds a new frontier in diabetic retinopathy therapy, harnessing the power of precision immunotherapy to correct ceramide imbalances at the molecular core of disease pathology. As the global burden of diabetes continues to escalate, innovations such as this are urgently needed to combat vision loss and improve outcomes.
This transformative approach not only reinvigorates hope for patients and healthcare providers but fundamentally reshapes our understanding of molecular interventions in chronic retinal diseases. Future investigations inspired by these findings are poised to redefine clinical standards and expand therapeutic horizons.
Subject of Research: Diabetic retinopathy and ceramide imbalance
Article Title: Reversing the effects of ceramide imbalance via anti-ceramide immunotherapy is an effective therapy for diabetic retinopathy
Article References:
Zhou, L., Li, J., Fu, C. et al. Reversing the effects of ceramide imbalance via anti-ceramide immunotherapy is an effective therapy for diabetic retinopathy. Cell Death Discov. (2025). https://doi.org/10.1038/s41420-025-02896-w
Image Credits: AI Generated