In recent years, the medical world has been witnessing significant advancements in the understanding of various forms of leukemia and their complications. Amongst these complexities, neuroleukemiosis stands out as a particularly rare yet crucial manifestation of acute myeloid leukemia (AML), especially in the pediatric population. The exploration of this condition represents a critical area of study that can significantly impact clinical practices in the diagnosis and management of leukemia in children.
Acute myeloid leukemia is an aggressive form of cancer that primarily affects the blood and bone marrow. Its prevalence in children, while less common than in adults, poses serious challenges to oncologists. Researchers have focused on how AML can present differently in young patients compared to adults. One area of particular concern is the potential for neurological complications, which can lead to severe morbidity and mortality if not diagnosed promptly.
Neuroleukemiosis refers to the infiltration of leukemic cells into the central nervous system, particularly the meninges and brain parenchyma. This condition can often be misdiagnosed or overlooked due to its subtle presentation and the varying symptoms that correlate with different stages of leukemia. Clinicians must be well-versed in recognizing these signs to facilitate early intervention, which can be pivotal in improving outcomes for affected children.
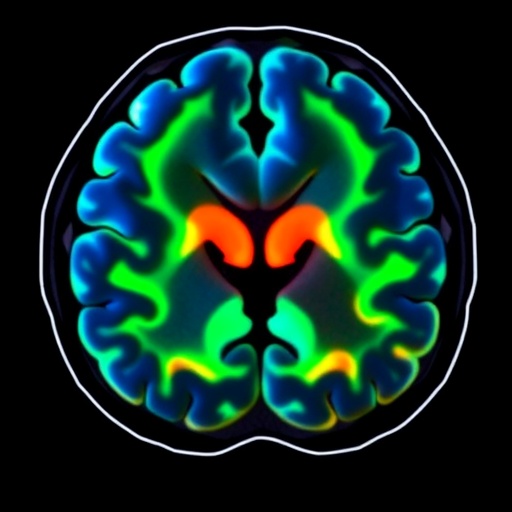
The imaging characteristics of neuroleukemiosis can exhibit a spectrum of presentations on modalities such as MRI and CT scans. Typically, MRI serves as the preferred imaging technique due to its superior ability to visualize the brain’s structures and potential abnormalities. Clinicians and radiologists should familiarize themselves with the imaging priors indicative of leukemic infiltration so that they can differentiate neuroleukemiosis from other more prevalent conditions, such as infections or other types of tumors.
In a recent scholarly article, the authors Dagar, Rahim, and Koehler delve into the specifics of neuroleukemiosis, detailing imaging characteristics and clinical presentations observed in young patients. Such studies are of paramount importance as they illuminate how neuroleukemiosis can represent a relapse of acute myeloid leukemia, offering a profound insight into the disease’s progression and associated complications.
The progression from initial diagnosis of AML to the manifestation of neuroleukemiosis can often be rapid and insidious. Symptoms typically include headaches, seizures, and altered mental status, which can mimic other underlying neurological disorders. These overlapping symptoms highlight the importance of a high index of suspicion among healthcare providers when managing young patients with a history of AML.
The loss of vigilance concerning neuroleukemiosis may also be attributed to the misconception that it seldom occurs in children. However, the truth is that this condition may be underreported due to the lack of awareness and comprehensive studies focusing exclusively on pediatric leukemia. Recognizing the potential for neuroleukemiosis is essential in ensuring prompt treatment, which can include intrathecal chemotherapy along with systemic treatments tailored to combat the underlying leukemia.
Moreover, understanding the biology of acute myeloid leukemia within the context of neuroleukemiosis is crucial for future research. Medical researchers are tirelessly working to unravel the genetic and molecular mechanisms driving leukemic infiltration into the central nervous system. This knowledge could ultimately lead to the development of more targeted therapies that not only focus on the systemic aspects of AML but also address the neurological implications.
As healthcare continues to evolve, collaboration between oncologists, radiologists, and neurologists becomes increasingly vital. An integrated approach to the treatment and management of pediatric leukemia patients with neurological manifestations ensures comprehensive care. Furthermore, fostering better communication channels among specialists can facilitate earlier detection and optimize treatment strategies for challenging cases such as neuroleukemiosis.
Educational initiatives aimed at increasing awareness of neuroleukemiosis among healthcare professionals are also essential. By improving educational curricula and fostering discussions in medical communities regarding the implications of this rare complication, the potential for early identification and the subsequent improvement of clinical outcomes can be enhanced.
In conclusion, neuroleukemiosis remains a significant complication associated with acute myeloid leukemia in children. Continued research, awareness, and education are crucial for refining diagnostic approaches and treatment modalities. As the understanding of leukemia advances, there is hope that innovative strategies will arise to effectively manage and mitigate the impact of such complex conditions on young patients and their families.
Subject of Research: Neuroleukemiosis as a manifestation of acute myeloid leukemia in children
Article Title: Neuroleukemiosis as a manifestation of relapse of acute myeloid leukemia in a child: imaging characteristics
Article References: Dagar, S., Rahim, M.Q., Koehler, S.M. et al. Neuroleukemiosis as a manifestation of relapse of acute myeloid leukemia in a child: imaging characteristics. Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06466-1
Image Credits: AI Generated
DOI: 02 December 2025
Keywords: Neuroleukemiosis, Acute Myeloid Leukemia, Pediatrics, Imaging Characteristics, Neurological Complications.