In the shadow of escalating global conflicts, the intersection of war and healthcare has become a critical concern, particularly for vulnerable populations with chronic illnesses. New research published in the International Journal for Equity in Health illuminates the alarming prevalence of malnutrition among patients with end-stage renal disease (ESRD) amid the turmoil of war in 2024. This investigative study, conducted by Elhassan and colleagues, offers a profound exploration into how war-induced disruptions exacerbate malnutrition in ESRD patients, with a focus on healthcare accessibility, gender disparities, dialysis availability, and economic inequalities.
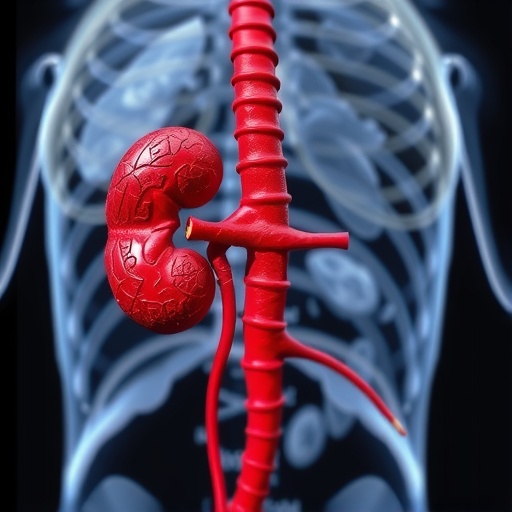
End-stage renal disease represents the terminal phase of chronic kidney disease, where kidney function is critically compromised, necessitating dialysis or transplantation. Malnutrition is a frequent yet often under-recognized complication in ESRD, directly impacting morbidity and mortality. The current conflict in 2024 has precipitated a humanitarian crisis, severely limiting healthcare infrastructure and access, thereby aggravating nutritional deficiencies among these patients. The study meticulously documents how interruptions in dialysis services, coupled with economic hardship and limited access to healthcare resources, culminate in a heightened malnutrition burden.
One of the pivotal revelations of this research is the stark disparity in nutritional status between genders. Women with ESRD in conflict zones experience disproportionately higher rates of malnutrition compared to their male counterparts. This phenomenon is attributed to entrenched socio-cultural norms that restrict women’s access to medical care and nutritional support, as well as economic dependencies exacerbated by war. The authors stress that addressing gender-specific barriers is imperative to implementing equitable healthcare interventions during wartime.
Healthcare access emerges as a critical determinant of nutritional outcomes in ESRD patients. The disruption of medical supply chains, destruction of healthcare facilities, and migration pressures during war significantly limit patients’ ability to maintain consistent dialysis treatment and receive nutritional counseling. The research highlights that even minimal interruptions in dialysis schedules can precipitate profound metabolic imbalances, thereby accelerating malnutrition and compromising patient survival.
Economic disparities further compound the challenge. The study presents a multidimensional analysis, correlating socioeconomic status with nutritional outcomes in ESRD patients. Individuals from impoverished backgrounds are more vulnerable, largely due to their inability to afford adequate nutritional supplements, access private healthcare, or maintain consistent dialysis treatment amidst systemic collapse. The authors argue that economic stratification during conflict not only reflects but deepens health inequities, creating a vicious cycle detrimental to patient care.
Dialysis, a lifesaving intervention for ESRD, becomes a logistical nightmare during war. Elhassan et al. elucidate how the scarcity of resources, damaged infrastructure, and security concerns impede the provision of regular dialysis. The irregularity and reduced frequency of treatments foster the accumulation of uremic toxins and exacerbate catabolic states, precipitating muscle wasting and nutritional deficits. The study underscores the necessity of innovative approaches to dialysis provision in conflict zones, such as mobile units or decentralized treatment centers.
The biochemical mechanisms underpinning malnutrition in ESRD are complex, involving inflammation, metabolic acidosis, hormonal imbalances, and anorexia. War-induced stress and trauma can intensify systemic inflammation, compounding nutritional deterioration. The research integrates clinical data demonstrating elevated inflammatory markers in malnourished ESRD patients during war, suggesting an interaction between psychosocial stressors and biological pathways driving cachexia and muscle protein degradation.
Importantly, the research critiques current nutritional assessment tools, emphasizing the need for conflict-adapted strategies. Standard indices like body mass index (BMI) and serum albumin levels may not fully capture malnutrition’s multifaceted nature in war settings. The authors advocate for comprehensive assessments incorporating dietary intake, inflammation markers, functional measures, and socioeconomic factors to tailor interventions effectively in resource-constrained environments.
The study’s policy implications resonate profoundly. Elhassan and colleagues call for urgent integration of nutritional support programs within emergency healthcare frameworks targeting ESRD populations. They propose collaboration between humanitarian organizations, local health authorities, and nephrology experts to develop sustainable interventions. Programs focusing on gender-sensitive approaches, economic assistance, and the restoration of dialysis continuity are deemed essential to mitigate malnutrition’s devastating impact.
Furthermore, the research highlights the significance of community engagement and health education. War zones often see the fragmentation of social networks; thus, empowering patients and caregivers through education about nutrition and home-based care may partially offset service gaps. The study highlights successful pilot programs that have leveraged local knowledge and resources to improve nutritional outcomes, advocating for their broader implementation.
The intersectionality of healthcare access, economic status, gender, and treatment availability forms the core analytical framework of this research. By employing a mixed-methods design that incorporates quantitative nutritional assessments and qualitative interviews with patients and providers, the study provides a comprehensive understanding of how these factors intertwine to shape malnutrition outcomes amid war. Such holistic insight is instrumental in crafting multifaceted interventions.
In addition to immediate clinical concerns, the research warns about the long-term public health consequences of unaddressed malnutrition in ESRD during conflicts. Prolonged nutritional deficits contribute to irreversible physical decline, increased hospitalizations, and substantial economic burdens on already strained health systems. Addressing malnutrition proactively is posited not only as a matter of survival but as a critical component of rehabilitation and post-conflict recovery.
This investigation stands as a clarion call to the international community. The authors emphasize that beyond political resolutions, there must be a parallel humanitarian commitment to safeguard the health of chronically ill populations caught in the crossfire. They advocate for the recognition of ESRD patients’ rights to uninterrupted, equitable healthcare access even amid warfare, highlighting the ethical imperatives involved.
Finally, the study contributes to a growing body of literature that situates non-communicable diseases within the context of humanitarian emergencies. By unraveling the intricate interplay of sociopolitical, economic, and biological determinants of malnutrition in ESRD patients during war, Elhassan et al. pave the way for future research and policy innovation. Their work challenges the global health community to rethink crisis response paradigms, ensuring inclusivity for vulnerable chronic disease groups.
In conclusion, this pioneering research exposes the hidden epidemic of malnutrition among ESRD patients in the war of 2024, underscoring the urgent need for integrated healthcare strategies that transcend conventional emergency responses. By highlighting gender disparities, economic challenges, healthcare access limitations, and dialysis disruptions, it paints a comprehensive picture of the multifactorial crisis. Its findings demand immediate action to protect the health and dignity of one of the most vulnerable patient cohorts in contemporary conflict zones.
Subject of Research: Malnutrition in patients with end-stage renal disease during war, focusing on healthcare access, dialysis, gender disparities, and economic inequalities.
Article Title: Malnutrition among patients with end-stage renal disease in war 2024: the role of healthcare access, dialysis, gender, and economic disparities.
Article References:
Elhassan, S., Abdelhadi, I.A.A., Mohamed, N.N.S. et al. Malnutrition among patients with end-stage renal disease in war 2024: the role of healthcare access, dialysis, gender, and economic disparities. Int J Equity Health 24, 298 (2025). https://doi.org/10.1186/s12939-025-02680-3
Image Credits: AI Generated