In the heart of East Sennar State, Sudan, a profound inquiry into the intersection of traditional medicine and modern healthcare sheds new light on the enduring challenge of mycetoma management. This neglected tropical disease, often overlooked in global health discussions, continues to burden impoverished communities with chronic disfigurement and disability. A recent qualitative study conducted by Elsheikh, Trueba, and Zaman dives deep into the local practices, beliefs, and healthcare-seeking behaviors surrounding mycetoma, highlighting the complex relationship between indigenous healing systems and conventional medical approaches.
Mycetoma, characterized by a persistent subcutaneous infection, often progresses to severe tissue damage and bone destruction if left untreated. Its management is notoriously challenging due to delayed diagnosis, limited access to healthcare facilities, and poor treatment compliance. In East Sennar State, where healthcare infrastructure is stretched thin, traditional healers play a pivotal role in addressing health concerns, filling gaps left by formal medical services. The study utilizes qualitative methodologies to unravel how traditional healing practices interface with biomedical interventions in the region.
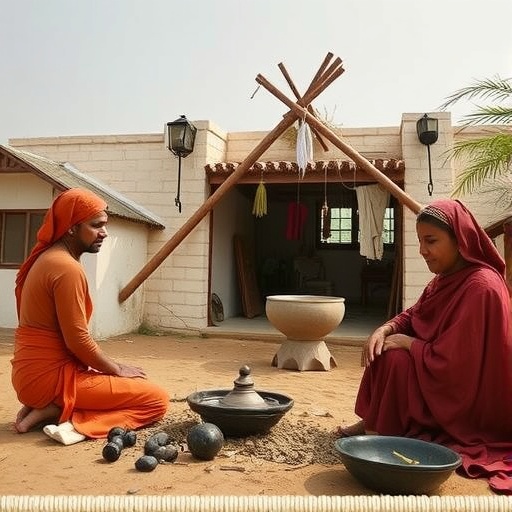
The researchers embarked on extensive fieldwork, engaging with affected patients, traditional healers, and healthcare professionals to gain an intimate understanding of the socio-cultural dimensions influencing mycetoma care. Their findings reveal a deeply entrenched trust in traditional healing modalities, often rooted in centuries-old knowledge systems that incorporate herbal remedies, spiritual rituals, and community-based support networks. Such practices not only serve therapeutic purposes but also foster culturally resonant frameworks for interpreting illness and suffering.
From a biomedical perspective, the study underscores critical obstacles to effective mycetoma treatment, including stigma associated with the disease and mistrust of modern healthcare providers. Many patients initially seek assistance from traditional healers due to geographical proximity, lower costs, and culturally congruent explanations of disease etiology. However, this delay in receiving biomedical treatment frequently results in disease progression, complicating clinical outcomes and necessitating more invasive interventions.
The synergy between traditional and modern healthcare systems offers a promising yet complex pathway for enhancing mycetoma management. The qualitative insights highlight potential avenues for integrative strategies that respect indigenous knowledge while emphasizing early diagnosis and adherence to antifungal therapies. Importantly, the study advocates for culturally sensitive health education campaigns that engage traditional healers as partners, promoting timely referrals and dispelling misconceptions about biomedical treatments.
Furthermore, the methodological approach employed by the researchers—emphasizing semi-structured interviews and thematic analysis—allows for a nuanced exploration of patient narratives. These narratives illuminate the lived realities of mycetoma sufferers, revealing the emotional and economic toll wrought by the disease. Many participants recount episodes of social exclusion and loss of livelihood, underscoring the urgent need for comprehensive care models that address not only clinical but also psychosocial dimensions.
This research also raises critical questions about the broader implications of integrating traditional healing within public health frameworks. It calls for policy dialogues that prioritize community engagement and capacity building among traditional practitioners, enabling them to function as effective agents in disease surveillance and management. Such policies could potentially redefine health equity paradigms by bridging gaps between marginalized populations and formal health systems.
Importantly, the study’s setting in East Sennar State presents unique environmental and socio-economic factors that influence disease dynamics. The endemic nature of mycetoma in this region correlates with factors such as agrarian livelihoods, climatic conditions favorable to the causative fungi, and limited healthcare infrastructure. These contextual variables underscore the necessity of localized interventions that tailor strategies to the distinct challenges faced by affected communities.
The research also touches upon the potential of technological innovations, such as mobile health platforms and digital diagnostics, to complement traditional healing networks. By harnessing technology to facilitate communication and monitoring, health systems could amplify the reach and effectiveness of integrated care models. This blending of technology and tradition might pave the way for scalable solutions in neglected tropical diseases beyond mycetoma.
Central to the findings is the recognition that successful mycetoma management transcends biomedical interventions alone. It necessitates a holistic approach that prioritizes cultural competence, patient empowerment, and systemic collaboration. By positioning traditional healers as critical stakeholders rather than peripheral actors, the study advocates for a paradigm shift that reconceptualizes healthcare delivery in resource-constrained settings.
Moreover, the research emphasizes the importance of sustained funding and international support to bolster mycetoma control efforts. Despite its severe impact, mycetoma remains underfunded and inadequately prioritized in global health agendas. Elevating the disease’s profile requires concerted advocacy that incorporates voices from affected regions and respects traditional healing’s role in community health resilience.
In examining the interplay between medical pluralism and disease management, the study offers vital lessons applicable to other neglected diseases and health conditions embedded in culturally rich contexts. It challenges researchers and practitioners to rethink reductionist approaches that ignore socio-cultural realities, urging a more inclusive, empathetic perspective that honors diverse healing traditions.
Ultimately, Elsheikh, Trueba, and Zaman’s work contributes to a growing body of evidence advocating for integrative health models where traditional knowledge systems and formal medicine converge to improve health outcomes. Their qualitative approach provides a roadmap for engaging communities in co-creating solutions that are medically sound, culturally appropriate, and socially just.
As the global health community grapples with the formidable challenge of reducing health disparities, understanding the nuanced dynamics explored in this study is critical. East Sennar State’s experiences underscore the transformative potential of harmonizing centuries-old healing wisdom with cutting-edge medical science—a synthesis that might hold the key to conquering mycetoma and similar neglected diseases worldwide.
Subject of Research: Traditional healing practices and mycetoma management in East Sennar State, Sudan.
Article Title: Traditional healing and mycetoma management in East Sennar State (Sudan): a qualitative exploration.
Article References:
Elsheikh, M., Trueba, M. & Zaman, S. Traditional healing and mycetoma management in East Sennar State (Sudan): a qualitative exploration. Int J Equity Health 24, 296 (2025). https://doi.org/10.1186/s12939-025-02641-w
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12939-025-02641-w