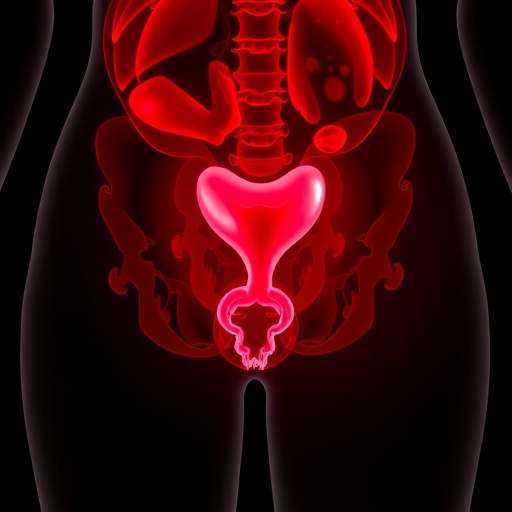
In a groundbreaking new study published in BMC Cancer, researchers have provided unprecedented real-world insights into the expression patterns and prognostic significance of two emerging molecular targets, trophoblast cell-surface antigen 2 (Trop-2) and folate receptor alpha (FRα), within the context of uterine carcinosarcoma (UCS). UCS represents a rare and highly aggressive subset of gynecological malignancies characterized by biphasic tumors that comprise both epithelial and sarcomatous components. The study addresses a critical gap in oncology by exploring biomarker prevalence that could ultimately guide precision therapies for this challenging disease.
Uterine carcinosarcoma has long posed therapeutic challenges due to its heterogeneity and poor prognosis. Conventional treatment typically involves surgical resection followed by a standardized chemotherapy regimen comprising carboplatin and paclitaxel, yet survival outcomes remain dismal. Biomarkers with therapeutic and prognostic relevance have been elusive, compounding the difficulty in tailoring treatment approaches tailored to individual tumors’ molecular profiles. This retrospective analysis analyzed UCS samples taken over nearly a decade, aiming to elucidate the landscape of Trop-2 and FRα expression and their correlation to patient outcomes.
The cohort consisted of 89 female patients diagnosed with UCS who underwent primary cytoreductive surgery followed by combination chemotherapy from 2012 through 2020. Using immunohistochemistry (IHC) on tissue microarrays, the investigators assessed the prevalence and intensity of Trop-2 and FRα in both epithelial and sarcomatous components. High Trop-2 positivity was stringently defined as strong staining intensity in 50% or more of tumor cells, whereas high FRα expression required medium-to-strong staining in 75% or more of cells. This rigorous scoring methodology ensured robust biomarker quantification and reliable downstream analysis.
Demographically, the mean age at diagnosis was 66.2 years, with a notable body mass index averaging 28.7 kg/m². Strikingly, over 70% of cases involved non-white women, illuminating potential racial disparities in UCS incidence or disease biology. Histopathologically, 63% of tumors showed heterologous sarcomatous differentiation, while lymphovascular invasion—a harbinger of metastatic spread—was seen in nearly 60% of cases. Importantly, surgeons achieved complete tumor resection (R0 margins) in just over two-thirds of patients, a factor later implicated as a pivotal prognostic determinant.
Regarding biomarker expression, high Trop-2 and FRα positivity was detected exclusively within the epithelial components of the tumors rather than the sarcomatous areas. Approximately 49.4% of epithelial components exhibited elevated Trop-2 expression, while markedly fewer—17.4%—demonstrated high FRα expression. Of particular note, FRα elevation correlated significantly with Trop-2 overexpression, suggesting potential co-regulation or shared pathways driving their upregulation in UCS epithelium.
Statistical analyses revealed key prognostic indicators. Patients with advanced stage disease or incomplete surgical resection experienced significantly shorter progression-free survival (PFS) and overall survival (OS), underscoring the paramount importance of early-stage diagnosis and aggressive surgical management. Multivariate models confirmed these findings, identifying both stage and resection status as independent predictors of poor outcomes. Additionally, lymphadenectomy was associated with improved survival, highlighting the potential therapeutic relevance of comprehensive nodal assessment.
Intriguingly, despite the promising prevalence data, neither Trop-2 nor FRα expression showed a direct association with worse or improved clinical outcomes in this cohort. This delineation implies that while these biomarkers are highly expressed, they may not function as independent prognostic factors in UCS. Nonetheless, their candidacy as therapeutic targets remains compelling given their membrane localization and involvement in tumor biology—features amenable to antibody-drug conjugates or receptor-targeted therapies currently in development.
The study’s findings have profound clinical implications. First, the demonstration of frequent Trop-2 overexpression aligns with emerging evidence in other aggressive carcinomas, where Trop-2-targeted agents such as sacituzumab govitecan have shown efficacy. Similarly, FRα-targeted therapeutics, including antibody-drug conjugates and folate-linked small molecules, offer a rationale for exploring precision medicine in UCS. The co-expression profile favors combination strategies or dual-targeting approaches, potentially overcoming tumor heterogeneity and resistance mechanisms.
From a molecular biology perspective, Trop-2 is a transmembrane glycoprotein implicated in cellular proliferation, migration, and invasion. Its dysregulation in epithelial malignancies associates with enhanced tumor aggressiveness and poorer prognosis in various cancers. FRα, a cell-surface receptor facilitating folate uptake, plays a critical role in nucleotide biosynthesis and cell division. Overexpression is linked to increased metabolic demands of rapidly proliferating tumors. Their membrane-bound nature makes both ideal candidates for targeted therapies exploiting antibody recognition to deliver cytotoxic payloads.
The lack of prognostic impact in this UCS cohort may reflect the complex tumor microenvironment and biology, where the interplay between epithelial and sarcomatous components dictates disease behavior. The study’s retrospective design and cohort size might also limit detection of subtle survival differences. Future prospective trials with larger populations and functional studies will be necessary to clarify the therapeutic potential and prognostic nuances of Trop-2 and FRα in UCS.
Overall, this research represents a critical step toward precision oncology for uterine carcinosarcoma. Complete surgical resection remains paramount for prolonging survival, emphasizing early detection and aggressive management. At the same time, identifying membrane protein targets prevalent in epithelial components offers new hope for biologically tailored treatments that could change the grim prognosis associated with this rare gynecologic malignancy.
The study highlights the need for multidisciplinary collaboration bridging surgical oncology, pathology, molecular biology, and pharmacology to translate these biomarker findings into effective clinical interventions. It also spotlights disparities in UCS affecting non-white women disproportionately, underscoring the importance of inclusive research efforts. As targeted therapeutics advance, integrating Trop-2 and FRα status into clinical decision-making algorithms for UCS could transform management paradigms.
In conclusion, the exploration of Trop-2 and FRα in UCS sheds light on tumor heterogeneity and molecular vulnerabilities. While neither marker predicted prognosis in this cohort, their high expression within epithelial tumor components and biologically relevant roles validate further investigation as therapeutic targets. Such breakthroughs promise to unlock novel, tailored therapies leading to improved outcomes in a cancer type historically resistant to conventional treatments.
Subject of Research: The prevalence and prognostic significance of trophoblast cell-surface antigen 2 (Trop-2) and folate receptor alpha (FRα) expression in uterine carcinosarcoma.
Article Title: Real-world insights into the prevalence and prognostic significance of trophoblast cell-surface antigen 2 and folate receptor alpha in uterine carcinosarcoma.
Article References:
de Albuquerque, L., da Silva, J., Rodrigues, F.R. et al. Real-world insights into the prevalence and prognostic significance of trophoblast cell-surface antigen 2 and folate receptor alpha in uterine carcinosarcoma. BMC Cancer (2025). https://doi.org/10.1186/s12885-025-15298-z
Image Credits: Scienmag.com