In a groundbreaking advancement poised to revolutionize hepatocellular carcinoma (HCC) treatment, researchers have unveiled a novel MRI-based deep learning model capable of accurately predicting early response to transarterial chemoembolization (TACE). Published in the 2025 volume of BMC Cancer, this multicenter study introduces a sophisticated analytical framework that integrates advanced imaging with clinical data, marking a transformative step towards personalized therapeutic decision-making for HCC patients.
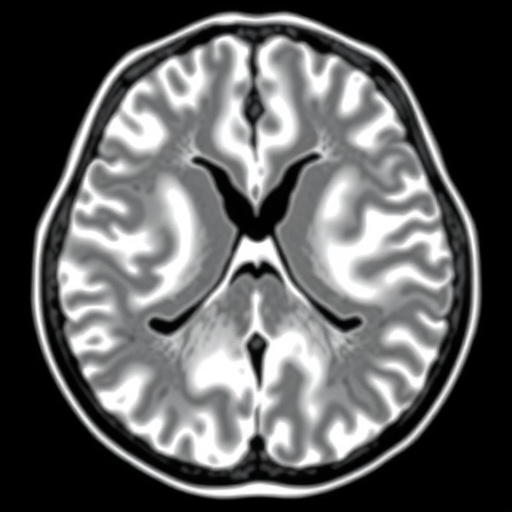
Hepatocellular carcinoma, the most common primary liver malignancy, often presents complex challenges due to its heterogeneous nature and variable response to conventional therapies like TACE. While TACE remains a stalwart intervention for intermediate-stage HCC, inconsistent treatment outcomes impede optimized clinical management. This newly developed algorithm addresses this critical gap by harnessing pretreatment magnetic resonance imaging (MRI) scans to forecast objective response to initial TACE, potentially sparing patients from ineffective interventions.
The research leverages retrospective datasets collated from three distinct medical institutions, encompassing a diverse cohort of HCC patients treated with TACE. Central to this effort is the creation of a deep learning framework, designated DLTR, that was meticulously compared against various competing algorithms to ascertain superior predictive performance. Building upon these foundations, the scientists incorporated a multilayer perceptron model, producing an enhanced classifier termed DLTR_MLP, which synergistically fuses imaging-derived features with pivotal clinical parameters.
Robust validation across multiple internal and external cohorts revealed the enhanced DLTR_MLP model exhibiting impressive discriminatory capability, measured via the area under the receiver operating characteristic curve (AUC). In external test sets, the model achieved AUC values as high as 0.818, substantially outperforming both the base deep learning algorithm and conventional clinical models. This marked increase underscores the algorithm’s potential reliability and applicability in real-world clinical settings across different geographical centers.
Notably, the model’s prognostic value extends beyond immediate treatment response. Survival analyses demonstrated the DLTR_MLP classifier’s aptitude for stratifying patients by progression-free survival, providing clinicians with insights into longer-term outcomes post-TACE intervention. Statistical evaluations with log-rank testing confirmed significant differentiation between survival curves, accentuating the clinical utility of integrating sophisticated imaging analytics into patient care algorithms.
Unraveling the biological implications underpinning these imaging signatures was a pivotal dimension of the study. Utilizing RNA-sequencing data sourced from The Cancer Imaging Archive (TCIA), the authors performed an intricate correlation analysis linking deep learning features extracted from MRI scans to gene expression profiles. This approach illuminated associations with 149 genes significantly linked to aggressive tumor biology pathways, such as angiogenesis, epithelial-mesenchymal transition (EMT), hypoxia, and transforming growth factor-beta (TGF-β) signaling.
The elucidation of these molecular pathways enriches our understanding of how imaging-derived biomarkers reflect underlying tumor proliferation and microenvironmental dynamics. For instance, the prominence of angiogenesis-related genes aligns with the vascular-centric mechanism of TACE therapy, which involves embolization of tumor-feeding vessels. Similarly, the identification of EMT and hypoxia pathways dovetails with established hallmarks of tumor invasiveness and therapeutic resistance, offering biological plausibility to the model’s predictive accuracy.
Integration of clinical variables with imaging features—realized through the DLTR_MLP model—demonstrates a notable enhancement in prediction robustness. Such multimodal analysis highlights the imperative of combining complex radiomic data with traditional patient metrics to fully capture the multifaceted nature of HCC progression and response to therapy. This fusion approach heralds a new era in precision oncology, wherein computational tools can enable clinicians to tailor interventions with unprecedented granularity.
From a technical standpoint, the deployment of a multilayer perceptron represents a sophisticated neural network methodology effective in handling nonlinear relationships inherent in heterogeneous datasets. This facet was critical in elevating model performance, facilitating nuanced interpretation of patterns embedded in high-dimensional MRI data alongside diverse clinical factors such as liver function tests and tumor staging.
Emphasizing external multicenter validation was a methodological strength of this investigation, addressing concerns of overfitting and enhancing generalizability across distinct patient populations. The consistency of results across geographically and demographically varied cohorts bolsters confidence in the potential for widespread clinical adoption of this model as a decision support tool in hepatology and oncology practices.
The implications of this research trajectory extend into clinical workflow integration. Incorporating the DLTR_MLP model within routine MRI analysis pipelines could provide oncologists with real-time predictive insights during pretreatment evaluations. Such early response prediction not only optimizes patient stratification but also aids in allocating healthcare resources more efficiently by identifying patients unlikely to benefit from standard TACE protocols.
Future prospects may include prospective trials designed to test the model’s predictive efficacy in real-time clinical decision-making scenarios, further refining its algorithms based on continuous data acquisition and performance feedback. Additionally, expansion of this approach to other liver-directed therapies or combined treatment modalities could broaden the scope of personalized treatment frameworks in HCC.
In essence, this deep learning-powered paradigm shifts the paradigm of HCC management towards precision medicine, illustrating how integrative computational analytics anchored in imaging and molecular biology can meaningfully augment clinical insights and therapeutic outcomes. The study’s innovative linkage between non-invasive imaging and tumor biology exemplifies the transformative potential of artificial intelligence applications in oncology.
As the burden of hepatocellular carcinoma continues to rise globally, particularly in regions with endemic liver disease, such advances are urgently needed to enhance survival rates and quality of life. By predicting which patients will respond favorably to TACE, this model empowers clinicians to tailor therapies more judiciously and dynamically, reducing unnecessary side effects and improving overall care standards.
This pioneering work exemplifies the convergence of radiology, bioinformatics, and clinical oncology, setting a new benchmark for future multidisciplinary research endeavors. The promise of merging high-dimensional MRI data with deep learning and gene expression profiling heralds an exciting frontier in cancer diagnostics and therapeutics.
Subject of Research:
Prediction of early treatment response to transarterial chemoembolization (TACE) in hepatocellular carcinoma using MRI-based deep learning models integrated with clinical data.
Article Title:
MRI-based deep learning model for early TACE response prediction in HCC: multicenter validation with biological insights
Article References:
Chen, M., Zhao, Z., Zhou, L. et al. MRI-based deep learning model for early TACE response prediction in HCC: multicenter validation with biological insights. BMC Cancer 25, 1810 (2025). https://doi.org/10.1186/s12885-025-15273-8
Image Credits: Scienmag.com
DOI: 24 November 2025