In the relentless pursuit of more effective cancer therapies, the tumor microenvironment remains one of the most formidable obstacles. Among the myriad challenges it presents, elevated interstitial fluid pressure (IFP) within tumors stands out as a critical barrier that restricts the penetration and efficacy of anticancer drugs. A groundbreaking preclinical study now sheds light on the promising potential of ultrasound-mediated microbubble (USMB) therapy to strategically modulate tumor IFP, thereby enhancing the delivery of drugs directly to malignant cells.
The study, carried out with meticulous animal model research involving VX2 tumors in New Zealand White rabbits, delved deeply into the spatial variability of tumor IFP and the dynamic influence of USMB treatment at multiple ultrasound pressure levels. The investigative team sought to unravel how adjusting ultrasound parameters might not only reduce the high interstitial pressures inherent in tumor cores but also how these adjustments impact the delicate balance of tumor perfusion—a vital element for successful drug transport.
Fundamentally, tumors generate elevated IFP due to their abnormal vasculature, dense extracellular matrix, and impaired lymphatic drainage. This heightened pressure hampers the influx of therapeutic agents, rendering conventional treatments less effective. The study’s use of the wick-in-needle (WIN) technique provided precise regional measurements, revealing a stark contrast between the tumor center and its peripheral zones. Central tumor regions exhibited significantly higher IFP values compared to the outer quarters, emphasizing the inherently heterogeneous landscape within tumors.
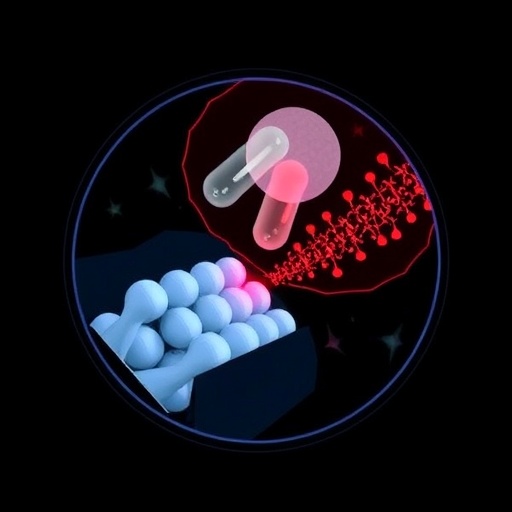
The dual role of USMB therapy emerges as both a mechanical and biological intervention. Microbubbles, when stimulated by focused ultrasound, exert localized mechanical forces that transiently disrupt tumor vasculature and cell structures. This disruption can lower IFP, potentially easing the passage of drugs into the tumor milieu. However, the extent and nature of this disruption depend critically on the applied ultrasound pressure, a factor the study meticulously varied across four levels: 1 MPa, 2 MPa, 3 MPa, and 5 MPa.
Intriguingly, the results indicated a nuanced relationship between ultrasound pressure and therapeutic outcomes. At moderate pressures of 2 MPa, USMB treatment achieved a noticeable reduction in IFP without significantly impairing tumor perfusion. This finding is particularly momentous as it suggests an optimized window where drug delivery can be facilitated by lowering interstitial resistance while preserving the vascular routes necessary for delivering those drugs.
Conversely, despite higher pressures of 3 MPa and 5 MPa producing even more pronounced decreases in tumor IFP, these levels also triggered substantial vascular damage. Contrast-enhanced ultrasound (CEUS) imaging and histological analyses revealed that such pressures caused extensive necrosis and disrupted the vascular integrity predominantly in the tumor core. This vascular destruction, although contributing to pressure reduction, paradoxically compromised perfusion—a critical detriment since it could ultimately impede drug transport to the tumor cells.
The study’s findings illuminate the critical importance of tailoring ultrasound parameters carefully. Too gentle a pressure might fail to sufficiently lower IFP, while overly aggressive settings risk obliterating the vascular pathways needed for therapeutic agents. This balance is pivotal when considering the complex physiology of tumors and the heterogeneity of microenvironmental pressures across different tumor regions.
The implications stretch beyond immediate therapeutic practice. USMB therapy introduces a sophisticated method to recalibrate the physical forces that govern drug access in solid tumors. Recognizing the discrete regional differences in tumor IFP underscores the need for personalized treatment planning, where ultrasound parameters are adjusted not just globally but with an understanding of the spatial complexities within tumors.
Moreover, such modulation of the tumor microenvironment could synergize with other treatment modalities. For instance, decreasing IFP might also enhance immune cell infiltration, potentially amplifying the effectiveness of immunotherapies. Hence, the integration of USMB with chemotherapeutic and immunomodulatory protocols offers compelling avenues for future research.
The careful ethical oversight and adherence to NIH animal care guidelines ensure that these insights rest on robust and responsible scientific foundations. The use of New Zealand White rabbits bearing VX2 tumors, a well-established model for solid tumors, lends translational relevance to human oncology.
Technologically, CEUS remains invaluable in this research domain, offering real-time visualization of perfusion changes that complement the quantitative IFP measurements. This convergence of imaging and biomechanical intervention constitutes a paradigm shift in tackling physical barriers to drug delivery.
The histological revelations of cellular and vascular damage at higher USMB pressures exemplify the fine line between therapeutic benefit and collateral injury. Understanding the threshold between modulating pressure to improve drug perfusion versus causing detrimental vascular disruption will be crucial for the clinical translation of this novel approach.
This study, therefore, carves out an exciting path for USMB therapy as a non-invasive, ultrasound-based intervention that directly addresses a core physical limitation of solid tumor treatment—the elevated interstitial fluid pressure. Through detailed measurement, imaging, and histological evaluation, it establishes a foundational understanding of how pressure modulation can be harnessed without undermining the vasculature essential for drug delivery.
In bridging the gap between engineering, oncology, and physiology, this research heralds a future where ultrasound parameters are meticulously tuned not only to maximize drug access but also to respect the intricate vascular balance within tumors. Such innovation could revolutionize the effectiveness of chemotherapy and other systemic treatments, turning physical barriers into therapeutic allies.
The quest to overcome solid tumors’ stubborn resistance gains a formidable new ally with USMB therapy. By tuning in to the tumor’s own microenvironmental pressures and employing ultrasound in an exquisitely targeted manner, science moves closer to a world where cancer treatments are more precise, effective, and personalized than ever before.
As further studies expand on these findings, attention will focus on optimizing protocols, understanding long-term effects, and integrating this technology with existing cancer treatment regimens. The promise of reducing tumor IFP while preserving perfusion signals a transformative step towards conquering the multifaceted challenges presented by the tumor microenvironment.
In essence, the battle against cancer is as much about overcoming the physical barricades within tumors as it is about targeting the malignant cells themselves. Ultrasound and microbubble technology, by bending these barriers, could redefine drug delivery and drastically improve patient outcomes in the near future.
Subject of Research: Tumor interstitial fluid pressure modulation using ultrasound and microbubble therapy in preclinical cancer treatment models.
Article Title: Modulating tumor interstitial fluid pressure using ultrasound and microbubble therapy: a preclinical study for enhanced drug delivery in cancer treatment.
Article References:
Chen, L., Liu, J., Chen, Q. et al. Modulating tumor interstitial fluid pressure using ultrasound and microbubble therapy: a preclinical study for enhanced drug delivery in cancer treatment. BMC Cancer (2025). https://doi.org/10.1186/s12885-025-15218-1
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-15218-1