In an ambitious and groundbreaking meta-analysis published in Translational Psychiatry in 2025, a team of neuroscientists led by Wang, Liu, and Zheng has unveiled a compelling narrative about the shared neural dysfunctions that underpin a spectrum of psychiatric disorders. Utilizing resting-state functional magnetic resonance imaging (fMRI), their work integrates findings across numerous independent studies to reveal commonalities in brain network abnormalities that may revolutionize our understanding and treatment of mental illness.
The complexity of psychiatric disorders has long posed challenges to researchers, clinicians, and patients alike. Diagnostic categories such as depression, bipolar disorder, schizophrenia, and anxiety disorders often present overlapping symptoms, making it difficult to delineate distinct neural correlates using traditional methods. Resting-state fMRI, which captures spontaneous brain activity fluctuations when subjects are not engaged in explicit tasks, has emerged as a powerful tool for identifying intrinsic functional connectivity patterns that reflect the brain’s baseline operational architecture. This meta-analysis synthesizes these patterns to find a converging neural signature across varied psychiatric conditions.
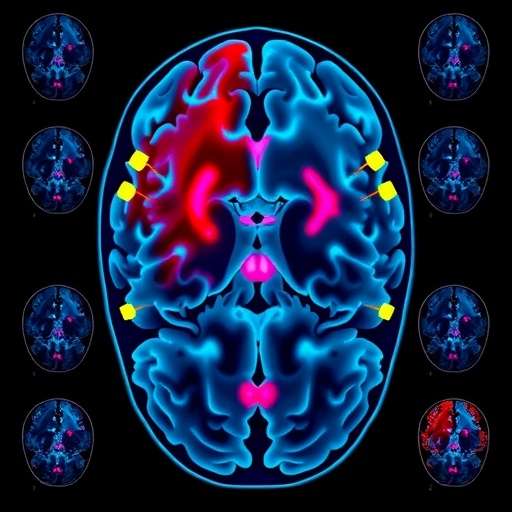
The researchers meticulously compiled data from dozens of resting-state fMRI studies, encompassing thousands of individuals with various psychiatric diagnoses alongside matched healthy controls. Through advanced statistical techniques and harmonized analytical frameworks, they examined alterations in connectivity within and between large-scale networks such as the default mode network (DMN), salience network (SN), and central executive network (CEN). These networks regulate self-referential thought, emotional salience, and cognitive control—the very pillars disrupted in mental illnesses.
One of the key revelations of the study is the consistent dysregulation observed in the DMN across psychiatric disorders. Typically active during rest and involved in introspection, self-referential processing, and memory, the DMN in affected individuals often shows hyperconnectivity or aberrant synchronization, which may contribute to rumination in depression or the distorted self-experience reported in schizophrenia. This finding aligns with theoretical models proposing that disrupted DMN activity underlies pervasive cognitive and affective symptoms.
Complementing these DMN changes, the salience network—which orchestrates attention and prioritization of relevant stimuli—was found to be hypoactive in several disorders. This hypoactivity compromises the brain’s ability to effectively flag emotionally significant environmental or internal cues, potentially leading to impaired emotional regulation and blunted affect seen in disorders like depression and schizophrenia. Altered connectivity within this network may also explain difficulties in shifting attention, a common cognitive deficit across psychiatric conditions.
Another critical insight is the variability found in the central executive network, responsible for higher-order cognitive functions such as working memory, decision-making, and cognitive flexibility. Across the psychiatric spectrum, reduced connectivity within the CEN was a frequent finding, suggesting a shared neural substrate for executive dysfunction. This impairment likely exacerbates challenges in planning, problem-solving, and impulse control, underscoring the neurocognitive symptoms that transcend diagnostic boundaries.
Importantly, the meta-analysis demonstrates that these network dysfunctions do not operate in isolation but reflect a broader imbalance in the brain’s functional architecture. The dynamic interactions between the DMN, SN, and CEN appear disrupted, flattening the adaptive switching mechanisms necessary for healthy cognition and emotion. The inability to transition smoothly between internally focused and externally directed processing modes may be a fundamental neural hallmark of psychiatric disease, offering a unified explanatory model.
This integrative perspective challenges traditional nosology, which treats psychiatric disorders as discrete entities. Instead, it supports a dimensional approach emphasizing transdiagnostic neurobiological mechanisms. Such a framework may inform the development of novel treatments targeting shared neural circuits rather than symptomatic labels, potentially improving therapeutic efficacy and reducing stigma linked to categorical diagnoses.
The authors also discuss the methodological advantages and challenges inherent in conducting a meta-analysis of resting-state fMRI data. Harmonizing studies with different imaging parameters, participant demographics, and preprocessing pipelines demands robust computational strategies. The authors utilized sophisticated meta-analytic techniques and validated them through sensitivity analyses, ensuring the robustness and reproducibility of their findings.
Future research directions suggested by the study include longitudinal investigations to assess how these network dysfunctions evolve over illness trajectories, treatment response, and recovery phases. Moreover, the integration of multimodal imaging data, combining structural MRI, diffusion tensor imaging, and electroencephalography, may provide a richer picture of the underlying neurobiology, advancing precision psychiatry.
The clinical implications of this meta-analysis are profound. By pinpointing convergent functional network abnormalities, clinicians may soon have access to reliable biomarkers that can refine diagnostic precision, monitor disease progression, and tailor interventions. Pharmacological, neuromodulatory, and behavioral therapies could be designed to recalibrate these dysregulated networks, ushering in an era of targeted neuropsychiatric care.
In addition to its translational impact, this work also energizes theoretical neuroscience by articulating a systems-level perspective of psychiatric vulnerability. The findings resonate with emergent concepts in network neuroscience emphasizing the brain’s modular yet integrated organization and how its disruption manifests in psychopathology.
Overall, Wang and colleagues’ meta-analysis represents a landmark effort to distill the vast and heterogeneous landscape of psychiatric neuroimaging into a coherent, actionable framework. Their identification of common neural dysfunctions across disorders is an important step toward demystifying the neurobiological substrate of mental illness, potentially sparking a paradigm shift in research and clinical practice.
As the mental health field grapples with rising prevalence rates worldwide, studies like this underscore the necessity of bridging basic neuroscience and psychiatry. By leveraging big data approaches and cutting-edge imaging techniques, researchers are poised to unlock the neural codes underlying psychiatric disorders, enhancing hope for affected individuals and families.
The fusion of advanced neuroimaging meta-analyses with integrative clinical models could redefine how mental illnesses are conceptualized and treated. It highlights the interdependence of brain networks in maintaining mental health, reinforcing the idea that optimal brain function arises from balanced connectivity rather than isolated regional activity.
This meta-analytic work stands as a clarion call for interdisciplinary collaboration spanning neuroscience, psychiatry, psychology, and computational sciences. Together, these fields can refine the neurobiological map of psychiatric disorders, translating complex brain patterns into practical clinical tools.
In conclusion, the discovery of common neural dysfunctions across psychiatric illnesses through resting-state fMRI meta-analysis offers a beacon of scientific hope. It invites a reconceptualization of mental health disorders not as fragmented conditions but as interconnected manifestations of fundamental brain network disruptions. Such insight holds tremendous promise for diagnosing, treating, and ultimately preventing psychiatric diseases more effectively.
Subject of Research: Neural dysfunction shared across psychiatric disorders identified via resting-state fMRI meta-analysis.
Article Title: Common neural dysfunction in psychiatric disorders: Insights from a meta-analysis of resting-state fMRI studies.
Article References:
Wang, L., Liu, Q., Zheng, Z. et al. Common neural dysfunction in psychiatric disorders: Insights from a meta-analysis of resting-state fMRI studies. Transl Psychiatry (2025). https://doi.org/10.1038/s41398-025-03760-2
Image Credits: AI Generated