Nestled between the stomach and spine, the pancreas plays a crucial role in regulating digestion and blood sugar levels within the human body. However, this vital organ can be afflicted by a particularly aggressive and lethal form of cancer known as pancreatic ductal adenocarcinoma (PDAC). PDAC is the predominant form of pancreatic cancer and ranks as the third leading cause of cancer-related mortality in the United States. Its insidious nature is underscored by its stealthy onset, making early detection challenging, and a daunting recurrence rate of approximately 70 percent post-treatment. Tragically, the survival statistics are grim, with only about 13 percent of those diagnosed surviving beyond five years.
At the University of Illinois Chicago, a multidisciplinary team consisting of surgeons, anesthesiologists, and engineers is making strides toward improving treatment outcomes for pancreatic cancer patients. Their groundbreaking research focuses on the impact of lidocaine, a widely used local anesthetic, on cancer cells shed into the bloodstream during surgical tumor removal. A recently published study in the journal Lab on a Chip describes novel advances in isolating these circulating tumor cells (CTCs) using innovative microfluidic technologies. This approach offers promising potential in mitigating metastatic spread during the vulnerable perioperative period.
Dr. Gina Votta-Velis, professor of anesthesiology at UIC College of Medicine and a principal investigator on the project, emphasizes the transformative potential of this research. Lidocaine, a mainstay in anesthesia for over six decades primarily for pain relief, may possess unrecognized anti-metastatic properties. Preliminary findings suggest that administering lidocaine intraoperatively could hinder the ability of CTCs to invade new tissues, thereby reducing the risk of cancer metastasis and ultimately enhancing patient prognoses.
In 2018, Dr. Votta-Velis secured funding from the American Society of Regional Anesthesia and Pain Medicine to explore this hypothesis. CTCs are cancer cells that detach from the primary tumor mass during surgery and enter systemic circulation. Their presence is strongly correlated with worse clinical outcomes and higher rates of tumor recurrence. Because these cells are exceedingly rare in blood compared to normal cells, capturing and studying them has remained a significant challenge in oncology.
Typically, patients must recover from surgery before commencing chemotherapy, creating a critical temporal window where CTCs can disseminate and seed secondary tumors. However, early in vitro experiments demonstrate that lidocaine may disrupt the ability of these cells to survive and exit the bloodstream. Instead, the anesthetic appears to facilitate their entrapment and subsequent clearance by immune cells. This innovative concept reframes lidocaine as not only an analgesic but also a potential agent to impede metastatic progression.
“Circulating tumor cells are essentially the seeds from which metastases grow,” explained Dr. Votta-Velis. “Identifying these cells and diminishing their virulence during critical treatment intervals offers an unprecedented approach to curtailing the metastatic cascade, which accounts for the majority of cancer-related deaths.” The implications for extending patient survival and quality of life could be profound.
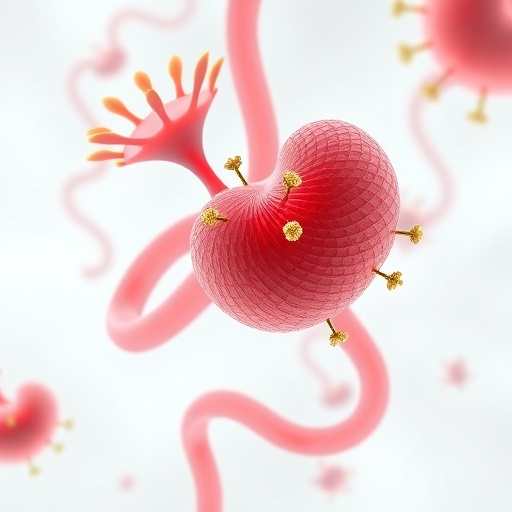
The rarity and heterogeneity of CTCs present formidable obstacles to accurate isolation and analysis. To overcome the proverbial “needle in a haystack” problem, the UIC team collaborated with Dr. Ian Papautsky, a biomedical engineering professor specializing in microfluidics—the manipulation of tiny fluid volumes through microscale channels. The team developed a novel microfluidic device composed of glass and plastic, measuring just a few inches and containing narrow channels only slightly wider than a human hair. This platform exploits size differences to separate larger, softer cancer cells from smaller blood components, facilitating a gentle, label-free liquid biopsy.
In 2019, Dr. Papautsky’s group demonstrated the device’s remarkable efficacy, achieving 93 percent accuracy in identifying CTCs without damaging them. In the latest work, they compared their microfluidic technique to the widely used EasySep system, which relies on magnetic bead-based cell separation. Unlike magnetic methods that can be harsh and compromise cell integrity, the microfluidic device retrieves significantly more viable cancer cells at greater speed—processing patient blood samples in as little as 20 minutes with an eightfold increase in recovery rate.
“Early and accurate detection of CTCs is indispensable for silent cancers like pancreatic cancer, where routine imaging often fails to identify disease progression,” said Dr. Papautsky. “Our device enables minimally invasive diagnostics, opening the door for personalized treatment strategies that target metastatic mechanisms at their earliest stages.” This technological innovation complements clinical efforts to intercept cancer dissemination before it culminates in full-blown metastasis.
Dr. Pier Giulianotti, co-investigator and chief of general, minimally invasive, and robotic surgery at UIC College of Medicine, echoed the significance of these findings. A globally recognized expert in pancreatic cancer surgeries, he highlighted that most malignant tumors metastasize via the bloodstream. “Understanding how cancer cells enter circulation and developing methods to control this phenomenon is not just important—it is essential to transforming how we manage aggressive cancers,” he stated.
The research team also comprises UIC scholars Celine Macaraniag, Ifra Khan, Alexandra Barabanova, Valentina Valle, and Alain Borgeat, as well as Jian Zhou from Rush University Medical Center. Together, they are forging a multidisciplinary path at the intersection of engineering, anesthesiology, and oncology, paving the way for therapies that could revolutionize pancreatic cancer treatment.
This pioneering effort exemplifies how integration of advanced microfluidic technologies with clinical research can yield transformative insights and novel interventions. While pancreatic cancer remains a formidable adversary, such innovative approaches to intercepting circulating tumor cells offer a glimmer of hope for improving survival rates and patient outcomes in what is often considered a high-mortality disease.
Subject of Research: The interaction of lidocaine with circulating pancreatic cancer cells and advancements in microfluidic isolation techniques.
Article Title: Lidocaine’s Potential to Inhibit Metastasis: Microfluidic Innovations in Pancreatic Cancer Treatment
News Publication Date: Not specified in source content.
Web References:
– U.S. Cancer Statistics: https://seer.cancer.gov/statfacts/html/common.html
– Pancreatic Cancer Survival Rates: https://seer.cancer.gov/statfacts/html/pancreas.html
– American Society of Regional Anesthesia and Pain Medicine: https://asra.com/news-publications/asra-updates/blog-landing/legacy-b-blog-posts/2021/01/29/past-carl-koller-memorial-research-grant-recipients
– Lab on a Chip Article DOI: http://dx.doi.org/10.1039/D5LC00512D
– Microfluidic Cell Separation Accuracy: https://www.nature.com/articles/s41378-019-0045-6
References:
Lab on a Chip, DOI: 10.1039/D5LC00512D
Image Credits: Photo by Sana Sheybanikashani, University of Illinois Chicago
Keywords: Pancreatic cancer, Microfluidics, Circulating tumor cells, Lidocaine, Metastasis, Liquid biopsy, Biomedical engineering, Cancer diagnostics