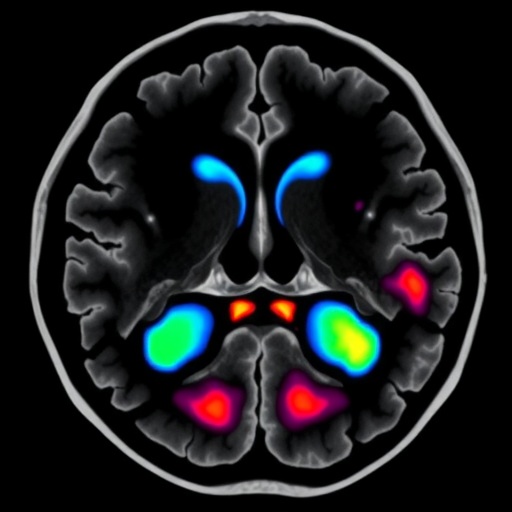
In a groundbreaking study poised to reshape prognostic evaluation in nasopharyngeal carcinoma (NPC), researchers have unveiled a novel muscle-specific MRI grading system that could significantly outpace traditional skull base invasion criteria in predicting patient outcomes. This retrospective analysis, encompassing nearly four hundred NPC patients treated with intensity-modulated radiotherapy (IMRT), provides compelling evidence that detailed assessment of soft tissue involvement (STI) via magnetic resonance imaging holds superior prognostic value, potentially heralding a paradigm shift in cancer staging and treatment planning.
Nasopharyngeal carcinoma, a malignancy arising from the epithelial lining of the nasopharynx, often presents diagnostic challenges due to its proximity to critical anatomical structures. Current staging largely hinges on bony skull base involvement and soft tissue spread patterns. The 9th edition of the AJCC/UICC staging system delineates T2 disease as soft tissue extension constrained within the lateral pterygoid (LP) muscle. Beyond this muscle, invasion into the masticator space or infratemporal fossa escalates the classification to T4, while bone erosion of the skull base is categorized as T3. However, this conventional approach, although clinically useful, may gloss over the nuanced biological behavior and prognostic diversity intrinsic to varying degrees and locales of muscle invasion.
The study, published in BMC Cancer, embarks on this frontier by dissecting the spectrum of soft tissue involvement with unprecedented specificity. Patients diagnosed between 2014 and 2019 underwent rigorous MRI examination, enabling the stratification of muscle invasion severity. The grading system classified STI on a continuum from mild — involving muscles like the tensor veli palatini or levator veli palatini — to moderate, marked by prevertebral muscle involvement, culminating in severe infiltration signified by medial or lateral pterygoid muscle or infratemporal fossa invasion. Complementing this, skull base invasion was grouped based on extent as limited or extensive.
Notably, the study’s survival analyses illuminate a striking correlation between the gradated muscle involvement and critical survival endpoints: local failure-free survival (LFFS), distant metastasis-free survival (DMFS), progression-free survival (PFS), and overall survival (OS). Over a median follow-up exceeding seven years, survival rates displayed a marked decrement aligned with progression from mild to severe STI. Patients with mild muscle involvement boasted an impressive five-year overall survival of 92.9%, whereas those with severe invasion faced a decline to just 68.0%. These gradations not only reached statistical significance with log-rank p-values below 0.0001 but also endured rigorous multivariate Cox proportional hazards modeling, underscoring their robustness as prognostic markers.
Perhaps most striking is the revelation that skull base bone erosion, a cornerstone of prior staging schemas, failed to demonstrate significant prognostic impact independent of muscle-specific grading. The lack of statistical association challenges entrenched dogma and advocates for a nuanced reevaluation of staging criteria. Indeed, the survival outcomes for patients with moderate muscle involvement and limited skull base invasion were nearly identical, corroborating the clinical relevance of muscle-specific stratification.
Beyond simply redefining prognostic frameworks, the findings bear direct therapeutic implications. The analysis identified induction chemotherapy as an independently protective factor, reducing mortality risk by approximately 45%, highlighting its role in tailored treatment strategies. This reinforces the intertwined nature of accurate staging and therapeutic decision-making, as precise risk stratification can guide the judicious use of aggressive systemic treatments.
The implications of this muscle-specific MRI grading extend beyond mere academic interest. In the era of precision oncology, where tailoring therapy to individual tumor biology is paramount, integrating such detailed imaging biomarkers may facilitate more personalized and effective treatment algorithms. Especially for NPC, a disease regionally prevalent yet globally challenging, these insights could influence clinical guidelines and improve survival outcomes worldwide.
Nevertheless, the authors prudently advocate for prospective, multi-institutional validation before widespread adoption. The retrospective design, while robust, necessitates confirmation in diverse patient cohorts and clinical settings to ensure reproducibility and generalizability. Such validation would cement the grading system’s utility and potentially transform international staging frameworks.
From a radiological perspective, this study underscores magnetic resonance imaging’s evolving role, transitioning from a mere diagnostic tool to a prognostic linchpin. The muscle-specific approach demands meticulous imaging protocol optimization and radiologist expertise to discern subtle variations in muscle infiltration, underscoring the convergence of technological advances and clinical acumen.
Moreover, this research exemplifies the iterative nature of cancer staging development, where anatomical understanding is continuously refined by clinical outcomes, imaging innovations, and molecular insights. By decoding the layered complexity of soft tissue invasion in NPC, scientists edge closer to demystifying tumor behavior and unlocking avenues for intervention that transcend traditional pathological boundaries.
The study’s extended follow-up duration—median 88 months—affords unparalleled insight into long-term outcomes, bolstering the relevance of the grading system for clinical prognostication. This temporal depth distinguishes the research from prior studies with shorter observation windows and enriches confidence in its conclusions.
Overall, this investigation invites the oncology community to reconsider entrenched paradigms and embrace refined imaging-driven staging criteria. If corroborated in future studies, muscle-specific MRI grading could become a new benchmark in NPC management, transforming diagnostic workflows and enhancing personalized patient care.
As nasopharyngeal carcinoma continues to impose a significant global health burden, such advances offer hope for improved survival and quality of life. By integrating radiological precision with clinical decision-making, researchers chart a promising course toward more effective, targeted therapies, ultimately reshaping NPC treatment landscapes.
In conclusion, the muscle-specific MRI grading system emerges as a powerful prognostic tool, outperforming traditional bone-focused criteria and enriching oncologic insight into soft tissue tumor spread. Its adoption may herald a new era in NPC staging, underscoring the indispensability of advanced imaging and nuanced anatomical assessment in modern cancer care.
Subject of Research: Prognostic evaluation of muscle-specific soft tissue involvement in nasopharyngeal carcinoma using MRI.
Article Title: Muscle-specific MRI grading of soft tissue involvement provides additional prognostic value beyond skull base criteria in nasopharyngeal carcinoma: a retrospective study.
Article References:
Yang, P., Liu, S., Chen, X. et al. Muscle-specific MRI grading of soft tissue involvement provides additional prognostic value beyond skull base criteria in nasopharyngeal carcinoma: a retrospective study. BMC Cancer 25, 1751 (2025). https://doi.org/10.1186/s12885-025-15208-3
Image Credits: Scienmag.com
DOI: 12 November 2025