In a groundbreaking advancement in neonatal cardiology and pulmonary medicine, new research has illuminated the crucial role of early left ventricular diastolic function impairment in the pathophysiology of congenital diaphragmatic hernia (CDH). This study brings to light the often overlooked cardiac dimension of this complex birth defect, especially highlighting how dysfunction in the left heart’s ability to relax and fill properly can contribute to severe respiratory complications. The implications are profound, offering potential for earlier diagnosis and tailored therapeutic approaches that address not only pulmonary issues but also underlying cardiac mechanisms.
Congenital diaphragmatic hernia, a malformation characterized by an incomplete formation of the diaphragm, allows abdominal organs to herniate into the chest cavity. This anatomical distortion exerts compressive forces on the developing lungs and heart, severely impairing function. While the pulmonary ramifications of CDH, including pulmonary hypoplasia and hypertension, have been extensively studied, the new evidence underscores how left ventricular (LV) diastolic dysfunction during the early transitional period after birth significantly exacerbates disease severity.
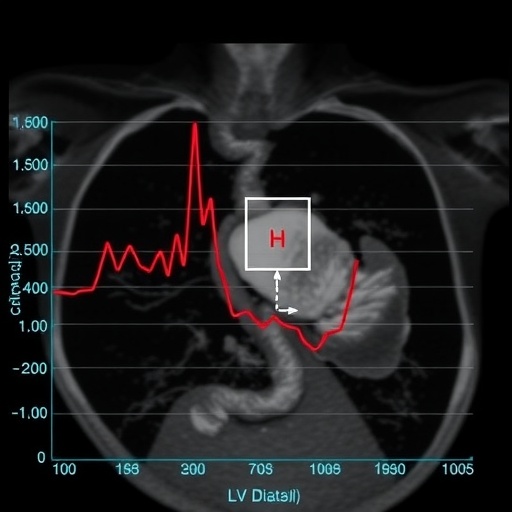
Diastolic function refers to the phase of the cardiac cycle when the heart muscle relaxes and the chambers fill with blood. In the context of congenital diaphragmatic hernia, the left ventricle may encounter increased stiffness or impaired relaxation, which compromises adequate filling. This dysfunction can precipitate elevated left atrial pressures, ultimately leading to post-capillary pulmonary hypertension. This form of pulmonary hypertension involves the backflow of pressure from the left side of the heart into the pulmonary circulation, a mechanism traditionally overshadowed by the more familiar pre-capillary causes linked to pulmonary vascular resistance.
This discovery has profound clinical implications. Neonates with CDH usually undergo extensive respiratory support, with the severity of pulmonary hypertension often dictating prognosis. However, this new understanding reveals that diastolic dysfunction in the left heart may independently or synergistically worsen pulmonary pressures and contribute to respiratory failure. Recognition of this mechanism asserts that treatment approaches must evolve beyond standard pulmonary vasodilators and ventilatory management to include strategies aimed at optimizing cardiac filling pressures and diastolic performance.
The researchers demonstrated that early echocardiographic assessment, specifically targeting detailed analysis of left ventricular diastolic function, can identify infants at heightened risk of adverse outcomes. Echocardiography, a non-invasive imaging technique vital for neonatal cardiology, allows assessment of key parameters such as mitral inflow velocities, tissue Doppler imaging, and left atrial size. These indices serve as surrogates for diastolic function and have been shown to correlate with the severity of pulmonary hypertension and gas exchange abnormalities in CDH patients.
Early identification of left ventricular diastolic impairment introduces a window of opportunity for clinicians to implement personalized therapies. For instance, the judicious use of pulmonary vasodilators, which aim to lower pulmonary artery pressures, must be balanced carefully to avoid exacerbating pulmonary congestion in the setting of poor left heart filling. Similarly, volume management through fluid boluses requires nuanced consideration, as excessive preload may overwhelm a noncompliant left ventricle, worsening pulmonary venous hypertension. Ventilatory strategies, particularly those utilizing higher airway pressures, might also be adjusted to minimize afterload on the left ventricle while ensuring adequate lung expansion.
The study’s predictions suggest that an integrated cardio-pulmonary monitoring approach during the critical transitional period—in the hours to days following birth—could significantly improve neonatal outcomes. Historically, neonatal management in CDH has primarily focused on respiratory support and stabilization, with less attention to detailed cardiac function beyond gross systolic performance. This pivot towards detailed diastolic function analysis represents a paradigm shift, advocating a more holistic understanding of cardio-pulmonary interplay.
From a mechanistic perspective, the impaired relaxation of the left ventricle in CDH is likely multifactorial. Chronic compression from herniated organs during fetal development leads to myocardial remodeling and fibrosis, altering intrinsic myocardial compliance. Furthermore, hypoplastic pulmonary vasculature and altered loading conditions at birth impose additional stresses on the left heart. These combined factors culminate in a stiff, poorly compliant ventricle incapable of accommodating necessary venous return, with downstream consequences on pulmonary pressures and oxygenation.
Clinicians and researchers alike are optimistic that these insights will spur innovation in both diagnostic and therapeutic domains. Echocardiographic indices of diastolic function could become routine components of neonatal cardiac evaluation in CDH, facilitating risk stratification and guiding nuanced management. Pharmacologic strategies targeting myocardial relaxation, possibly involving novel agents or repurposed drugs, may emerge as adjuncts in comprehensive treatment regimens. Additionally, ventilatory techniques might be refined to lessen hemodynamic compromise linked to left ventricular diastolic dysfunction.
Understanding the precise temporal evolution of these cardiac changes is another exciting frontier. The early transitional period after birth encompasses dramatic physiological shifts in pulmonary and systemic circulation, placing dynamic demands on cardiac performance. Longitudinal studies focusing on diastolic function trajectories in CDH infants could clarify optimal timing for interventions and identify critical thresholds predictive of deterioration or recovery.
In this context, the role of post-capillary pulmonary hypertension redefines our grasp of pulmonary vascular disease in CDH. Unlike traditional pre-capillary pulmonary hypertension—characterized by heightened pulmonary vascular resistance—post-capillary hypertension reflects elevated pressures from the heart’s inability to adequately manage pulmonary venous return. Therapeutic strategies designed to selectively target this hemodynamic subset might yield better clinical responses and reduce mortality associated with CDH.
The integration of these novel insights also necessitates education and training for neonatologists, cardiologists, and intensivists, ensuring broad awareness of diastolic dysfunction’s contribution and fostering multidisciplinary collaborations. Enhanced echocardiographic training to interpret nuanced diastolic parameters will be essential, alongside development of clinical protocols balancing respiratory, hemodynamic, and cardiac considerations.
Importantly, this research underscores that congenital diaphragmatic hernia is not merely a respiratory disease but a complex cardio-pulmonary syndrome necessitating comprehensive evaluation and tailored care strategies. The findings may also inspire investigations into similar cardiac contributions in other neonatal conditions characterized by pulmonary hypertension and compromised oxygenation.
Ultimately, the hope is that embracing early left ventricular diastolic function as a pivotal factor in CDH pathophysiology will translate into improved survival rates and quality of life for affected infants. As research and clinical practice evolve, this integrated approach may herald a new era in the management of this challenging congenital disorder, transforming outcomes through precision medicine.
In conclusion, the study marking a significant milestone in understanding CDH offers a compelling case to revisit longstanding assumptions about neonatal pulmonary hypertension. It repositions left ventricular diastolic dysfunction at the heart of disease severity and clinical outcomes, advocating for early, detailed cardiac assessment and individualized management to better navigate the critical transitional period.
Subject of Research: Left ventricular diastolic function and its impact on disease severity in congenital diaphragmatic hernia.
Article Title: Early left ventricular diastolic function and disease severity in congenital diaphragmatic hernia.
Article References:
Cantone, G.V., Bhattacharya, A., Healy, D. et al. Early left ventricular diastolic function and disease severity in congenital diaphragmatic hernia. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04560-6
Image Credits: AI Generated
DOI: 12 November 2025