In a groundbreaking advancement in pancreatic cancer surveillance, researchers at Johns Hopkins Medicine have identified mild dilation of the pancreatic duct as a critical early indicator of pancreatic ductal adenocarcinoma (PDAC) risk in high-risk individuals. Published in the November 2025 issue of Gastro Hep Advances, the study illuminates how subtle structural changes detectable through imaging modalities could revolutionize early detection of a disease notoriously elusive in its initial stages.
Pancreatic ductal adenocarcinoma, predicted by the National Institutes of Health to become the second-leading cause of cancer mortality in the United States by 2030, presents formidable challenges due to its asymptomatic nature in early phases and aggressive progression. Current surveillance guidelines, endorsed by influential bodies such as the International Cancer of the Pancreas Screening (CAPS) Consortium and the American Society for Gastrointestinal Endoscopy, recommend vigilant monitoring for individuals with significant familial or genetic predispositions. Yet, despite these protocols, catching tumors while still localized has been persistently difficult.
This Johns Hopkins-led research emerged from the CAPS Study, a long-term prospective cohort investigation initiated in 1998, meticulously following individuals at elevated risk for PDAC due to genetic or familial factors. Through routine surveillance using endoscopic ultrasound (EUS) and magnetic resonance imaging (MRI), investigators measured the diameter of participants’ pancreatic ducts, uncovering a compelling correlation: a duct diameter exceeding four millimeters markedly elevated the likelihood of neoplastic progression, including high-grade dysplasia and invasive cancer.
Out of 641 high-risk participants evaluated, 97 demonstrated pancreatic duct enlargement absent any mass lesion obstructing the duct, a subtlety previously undervalued in clinical risk assessments. Among these individuals, ten experienced progression to neoplasia within a median timeframe of two years after the initial detection of duct dilation. Remarkably, the cumulative probability of developing pancreatic cancer in patients with baseline duct widening reached 16% at five years and soared to 26% at the ten-year mark, underscoring the prognostic significance of this anatomical change.
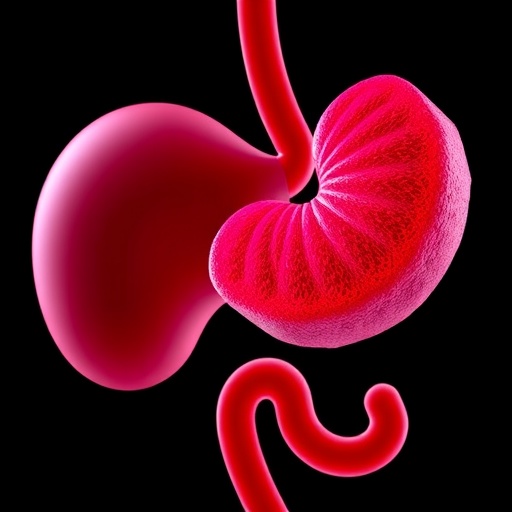
The pathophysiological implications of this finding are profound. Even when the primary tumor mass evades visualization due to size or location limitations, the pancreatic duct’s mild dilatation serves as a sentinel biomarker of underlying malignant transformation. This phenomenon highlights the duct’s role not merely as a passive conduit but as a dynamic structure whose alterations presage disease progression at a microscopic level.
Dr. Marcia Irene Canto, the study’s lead investigator and a professor of medicine and oncology at Johns Hopkins University School of Medicine, emphasizes the transformative potential of recognizing duct dilation as a red flag. By detecting risk earlier, clinicians gain a crucial window for intervention—whether through surgical resection or escalated imaging frequency—potentially improving survival outcomes for patients predisposed to this lethal malignancy.
Beyond EUS and MRI, the implications extend to other imaging modalities as well. Ductal dilatation, if identified incidentally during computed tomography (CT) scans performed for unrelated conditions such as abdominal pain or renal calculi, could prompt timely referral for specialized pancreatic evaluation. This broadens the horizons for opportunistic screening and suggests a paradigm shift in how incidental pancreatic findings are interpreted in high-risk populations.
Adding a futuristic dimension, the research team is exploring the integration of artificial intelligence (AI) algorithms capable of synthesizing imaging data with clinical parameters to refine risk stratification. This technological synergy aims to enhance predictive accuracy, reduce false positives, and individualize surveillance strategies, propelling precision medicine into the realm of pancreatic oncology.
The meticulous nature of this research is also reflected in its multidisciplinary collaboration, encompassing radiologists, oncologists, gastroenterologists, and molecular pathologists. Contributors such as Drs. Elizabeth Abou Diwan, Helena Saba, Amanda L. Blackford, and others collectively enriched the investigation with their diverse expertise, reinforcing the necessity of comprehensive approaches in confronting pancreatic cancer.
Funding for this pivotal study was robust and multifaceted, deriving from NIH grants alongside contributions from philanthropic entities such as the Susan Wojcicki and Dennis Troper Foundation and the Stand Up to Cancer-Lustgarten Foundation Pancreatic Cancer Interception Translational Cancer Research Grant. Additional support stemmed from the Pancreatic Cancer Action Network, the Rolfe Pancreatic Cancer Foundation, and other dedicated organizations committed to advancing understanding and treatment of this devastating disease.
Importantly, the study’s disclosures maintain transparency regarding potential conflicts of interest. Dr. Canto’s consultancy roles and royalties are openly acknowledged, ensuring the integrity of the research findings. Most other authors report no conflicts, highlighting the study’s adherence to rigorous ethical standards.
This revelation about pancreatic duct dilation not only enriches the clinical toolkit for managing high-risk cohorts but also underscores the critical importance of vigilant and nuanced imaging interpretation. As pancreatic cancer’s grim mortality statistics loom large, such incremental advances offer glimmers of hope. Early identification and timely intervention could soon shift the prognosis paradigm, transforming a typically fatal disease into a manageable condition.
In summary, the identification of mild pancreatic duct dilation as a harbinger of neoplastic transformation represents a landmark insight in early pancreatic cancer detection. This finding, corroborated by extensive longitudinal surveillance, promises to refine screening protocols, facilitate early therapeutic engagement, and ultimately improve patient survival. With advances in imaging technology and AI-driven analytics on the horizon, the fight against pancreatic cancer may be entering a new, more hopeful era.
Subject of Research: Early detection markers and surveillance of pancreatic ductal adenocarcinoma in high-risk individuals.
Article Title: Identifying Pancreatic Duct Dilatation as a Crucial Early Risk Factor in High-Risk Surveillance Cohorts
News Publication Date: November 2025
Web References:
References:
- National Institutes of Health, Pancreatic Cancer Statistics and Projections
- Johns Hopkins CAPS Study Publications
- Gastro Hep Advances, November 2025 Issue, Volume X, Article ID S2772-5723(25)00189-X
Image Credits: Marcia Canto
Keywords: Pancreatic cancer, pancreatic ductal adenocarcinoma, early detection, endoscopic ultrasound, pancreatic duct dilation, imaging biomarkers, cancer surveillance, longitudinal cohort study, artificial intelligence, genetic risk, high-risk screening, neoplastic progression