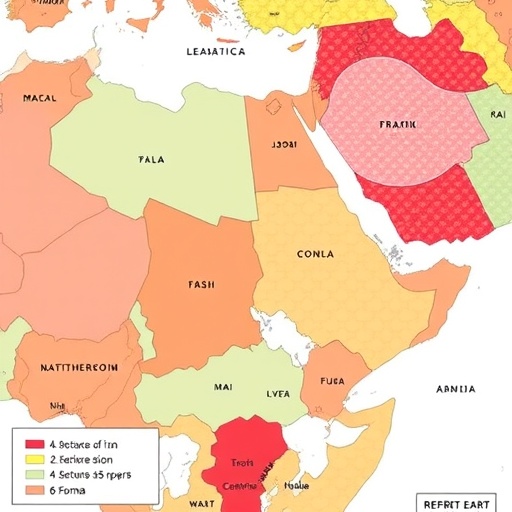
Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) is rapidly emerging as a formidable health burden across the Middle East and North Africa (MENA) region, yet the healthcare infrastructure and policy landscapes remain rudimentary and fragmented. Recent comprehensive research surveying 17 countries within this diverse region has illuminated critical systemic gaps hampering effective MASLD management. These findings underscore the urgency of overhauling current models of care by embedding integrated national strategies, enhancing clinical pathways, and galvanizing multidisciplinary collaboration to combat this escalating liver health crisis.
At its core, MASLD epitomizes a complex liver pathology intimately linked to metabolic disturbances, including obesity, insulin resistance, and type 2 diabetes—conditions whose prevalence is surging throughout the MENA region. Despite this troubling epidemiological trend, the study reveals the absence of robust national clinical guidelines in nearly two-thirds of the surveyed nations, which significantly hampers standardized care delivery. This deficiency in strategic direction creates a landscape where medical interventions remain inconsistent, and clinical outcomes variable, often to the detriment of patient prognosis.
The investigative team deployed a rigorous, mixed-methods approach, engaging 130 healthcare specialists spanning academia, public hospitals, and private sectors. This methodology afforded a multidimensional perspective on existing MASLD care models, encapsulating diagnostic capabilities, treatment avenues, referral mechanisms, and educational outreach. Such broad representation ensures the findings reflect real-world practices and challenges, offering a credible blueprint to catalyze systemic reform.
One of the most glaring deficits unearthed is the paucity of structured referral systems, with barely 40% of practitioners confirming their existence. This fragmentation contributes to delays in diagnosis and treatment initiation, exacerbating disease progression. Moreover, clinical infrastructure disparities are starkly apparent; advanced diagnostic modalities like transient elastography—a non-invasive technique pivotal for fibrosis assessment—remain accessible to only a quarter of providers. This technological shortfall impedes early detection and risk stratification, critical determinants of therapeutic success.
Multidisciplinary team (MDT) integration, recognized globally as best practice in managing chronic liver diseases, is acknowledged by 60% of clinicians as valuable. Yet, real-world implementation is sporadic and inconsistent across the surveyed region. The suboptimal institutionalization of MDT care reflects broader systemic challenges, including resource constraints, limited cross-specialty collaboration, and insufficient policy mandates. Addressing these structural barriers is paramount to harnessing the collective expertise needed for comprehensive MASLD management.
Public engagement and patient-centered strategies represent another dimension requiring urgent attention. The study indicates that public education efforts are minimal; over 20% of respondents report an alarming absence of educational tools targeting MASLD awareness. Furthermore, a staggering 87.7% noted a lack of patient-reported outcome metrics, impeding nuanced understanding of disease burden and treatment impact from the patient perspective. Enhancing awareness is crucial not only to improve adherence—which nearly half of respondents identify as poor due to low awareness and financial hurdles—but also to empower patients to engage proactively in their care journey.
Policy-level analysis paints a sobering picture. The majority of nations lack comprehensive national MASLD control strategies, reflecting a broader inertia in healthcare planning for metabolic diseases. This policy vacuum mirrors insufficient allocation of resources, inadequate health workforce preparation, and the absence of incentive frameworks that prioritize chronic liver disease management within health systems traditionally focused on communicable diseases or acute care.
The complexity of MASLD, which traverses metabolic, hepatic, and cardiovascular domains, demands an integrated, multisectoral response. Strengthening health system capacity involves not only augmenting clinical infrastructure but also investing in healthcare professional education, standardizing care algorithms, and establishing interoperable data systems for surveillance and research. These elements collectively foster an environment conducive to evidence-based, timely interventions.
Beyond medical and infrastructural enhancements, the study advocates for a paradigm shift emphasizing holistic health system preparedness. This includes the adoption of coordinated care models embedding hepatologists, endocrinologists, dietitians, and primary care providers within MDTs capable of delivering personalized treatment plans and sustained patient follow-up. Such models have the potential to improve clinical outcomes, optimize resource use, and ultimately mitigate the growing MASLD-related morbidity and mortality.
The solutions proposed extend to developing and institutionalizing national clinical guidelines reflective of the latest scientific evidence and region-specific epidemiological data. Embedding these guidelines within healthcare policies can catalyze uniformity in diagnostic criteria and therapeutic approaches, ensuring equitable care across the heterogeneous MENA region. Moreover, fostering public-private partnerships could play a pivotal role in scaling up access to advanced diagnostics and therapeutics.
Importantly, the voice of frontline clinicians captured in this research signals a readiness within the medical community to champion and drive systemic changes. Their insights delineate pragmatic steps, from enhancing multidisciplinary collaboration to expanding educational campaigns, that stakeholders can harness to build momentum for transformative health policies.
In conclusion, the escalating MASLD epidemic across the MENA region presents a multifaceted challenge demanding concerted action, transcending conventional medical interventions. The study’s comprehensive mapping of care models unambiguously highlights structural, educational, and policy deficiencies that obstruct effective management. Bridging these gaps through integrated strategy formulation, infrastructural investment, and robust public engagement stands as a critical imperative for safeguarding liver health amidst evolving metabolic challenges. The urgency of this call to action is matched only by the opportunity to effect lasting, impactful change in a region on the precipice of a metabolic health crisis.
Subject of Research: Metabolic Dysfunction-associated Steatotic Liver Disease (MASLD) care systems in the Middle East and North Africa (MENA) region
Article Title: Mapping Metabolic Dysfunction-associated Steatotic Liver Disease Models of Care across 17 Middle East and North Africa Countries: Insights into Guidelines, Infrastructure, and Referral Systems
News Publication Date: 1-Sep-2025
Web References:
- Journal of Clinical and Translational Hepatology: https://www.xiahepublishing.com/journal/jcth
- DOI: http://dx.doi.org/10.14218/JCTH.2025.00286
Image Credits: Mohamed El-Kassas
Keywords: Steatohepatitis, Metabolic disorders, Fatty liver disease, MASLD, MENA region, Liver disease management, Multidisciplinary care, Transient elastography, Public health policy, Clinical guidelines