Between 2012 and 2022, the United States witnessed a troubling escalation in premature mortality among adults aged 18 to 64. Contrary to expectations of medical advancements and improved public health initiatives, premature death rates rose sharply by over 27% across this demographic. This stark increase signals a profound reversal in the trajectory of health outcomes among working-age adults and exposes underlying fractures within the nation’s health systems and societal structures.
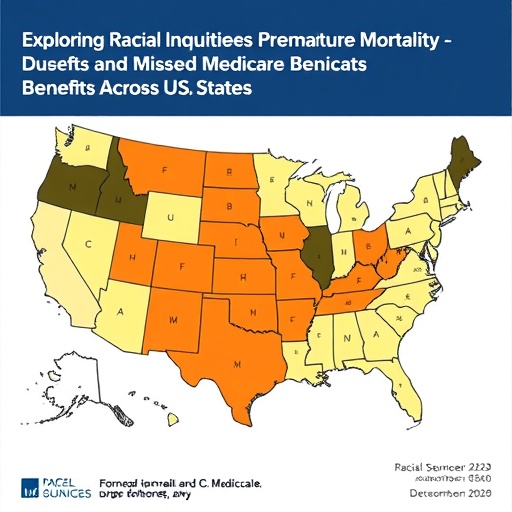
A particularly alarming dimension of this trend is the exacerbation of racial disparities in premature mortality. Throughout the decade, Black individuals consistently suffered from higher rates of premature death compared to their white counterparts. Not only did these disparities persist, but they also widened significantly across most states. This indicates systemic and entrenched health inequities that cut across geographic boundaries, implicating broader socio-economic and structural factors rather than localized or temporary issues.
The data underline a critical paradox in the U.S. healthcare entitlement system, especially relating to Medicare. Medicare, a federal program primarily designed to serve Americans aged 65 and older, depends on contributions made by individuals during their working years. However, many Black Americans do not live long enough to qualify for this essential coverage, despite decades of labor and financial input into social insurance programs. This premature mortality crisis thus not only reflects health inequities but also signals a fundamental injustice in the financing and distribution of healthcare benefits.
Structural inequities within healthcare access, quality, and financing contribute heavily to this phenomenon. Social determinants of health—including economic instability, educational disparities, environmental exposures, and systemic racism—intersect to influence mortality patterns. These factors shorten life expectancy for Black individuals, while also limiting access to preventive care and effective treatments during critical life stages. Such inequities perpetuate cycles of poor health, ultimately manifesting in increased premature deaths.
The impact of these mortality trends extends beyond individual health outcomes, affecting community stability and economic productivity. Premature death in working-age adults leads to a loss of economic contributions, increased burdens on social and healthcare services, and diminished intergenerational wealth. Moreover, the disproportionate burden borne by Black communities exacerbates existing social inequalities, deepening divides that challenge societal cohesion and equity.
This shift in mortality also raises critical questions about the adequacy of current health insurance structures, particularly those tied to employment and age. Given that Medicare eligibility starts at age 65, the rising mortality before this age leaves many without coverage during vulnerable years. This gap indicates a need for policy reform aimed at more equitable access to health insurance and care, perhaps by rethinking entitlement frameworks or expanding coverage eligibility to better serve marginalized populations.
Analyzing mortality data from multiple states reveals that while premature deaths increased across the board, the most severe escalations were localized within communities grappling with concentrated poverty, limited healthcare infrastructure, and persistent racial segregation. Geographic disparities intertwine with racial inequities, suggesting that interventions must be geographically as well as demographically tailored to effectively address the crisis.
Racial differences in mortality rates also underscore the role of chronic health conditions disproportionately affecting Black adults, including hypertension, diabetes, and cardiovascular diseases. These conditions, often rooted in long-term social and economic deprivation, contribute significantly to premature mortality. The heightened prevalence and worsened outcomes of such diseases among Black populations necessitate targeted public health strategies focusing on prevention, early detection, and sustained management.
The increasing premature mortality trend in the U.S. contradicts the overall global progress in life expectancy and health improvement seen in many developed countries. This divergence highlights the unique challenges faced by the U.S., including fragmented healthcare delivery, inequitable access, and entrenched social disparities. Understanding and reversing these trends demand multifaceted solutions integrating health policy reform, community engagement, and socioeconomic improvements.
Researchers emphasize that addressing this mortality gap requires confronting the root causes embedded within structural racism and economic inequality. Interventions that focus solely on medical care without addressing social determinants are unlikely to achieve substantial progress. A comprehensive approach necessitates cross-sector collaboration among healthcare providers, policymakers, and community organizations to dismantle barriers and foster equitable health environments.
Moreover, this mortality pattern carries implications for national entitlement programs and the future sustainability of healthcare financing. As premature mortality siphons away a vital segment of the workforce before age 65, the funding base for Medicare and similar programs may become increasingly unstable. This dynamic adds urgency to policy discussions about healthcare coverage, social safety nets, and preventive public health investments aimed at extending healthy lifespan.
The research team led by Irene Papanicolas, PhD, from Brown University, calls for an urgent re-examination of Medicare and health policy frameworks to better reflect the realities of racial health disparities and premature mortality. Only by integrating equity-focused approaches in health insurance design and social policies can the nation hope to mitigate this growing crisis, ensuring that all Americans can enjoy longer, healthier lives and equitable access to essential healthcare services.
Subject of Research: Premature mortality trends and racial disparities in the United States adult population aged 18 to 64 from 2012-2022, with implications for Medicare entitlement and health equity.
Article Title: (doi:10.1001/jamahealthforum.2025.4916)
Keywords: Mortality rates, Racial differences, United States population, Age groups, Health insurance, Life expectancy, Life span, Ethnicity