In recent years, malignant melanoma has persisted as one of the deadliest forms of skin cancer, continuously challenging researchers and clinicians alike due to its aggressive progression and frequent resistance to conventional therapies. The complexity of melanoma, especially its interaction within the tumor microenvironment, calls for sophisticated and reliable models that can accurately replicate human skin and tumor biology. Traditional two-dimensional (2D) cell cultures and even standard three-dimensional (3D) systems such as spheroids and organoids, though useful, fail to comprehensively simulate the multi-layered, vascularized, and immunologically active environment of native skin. This gap has driven the development of advanced platforms, among which 3D bioprinting emerges as a revolutionary technology enabling the precise construction of melanoma models that hold promise for both understanding tumor dynamics and screening innovative therapies.
3D bioprinting harnesses the power of additive manufacturing, allowing researchers to spatially arrange various cell types and extracellular matrix components with remarkable accuracy. This innovation ensures that printed melanoma models more faithfully mirror the cellular heterogeneity and complex architecture of native human skin. By integrating multiple bioinks, each designed to emulate different aspects of skin biology, these bioprinted constructs achieve remarkable biomimicry. This approach provides a critical advantage over previous models by incorporating vascular-like structures and even elements of immune system components—features that are pivotal in modulating tumor behavior and therapeutic responses.
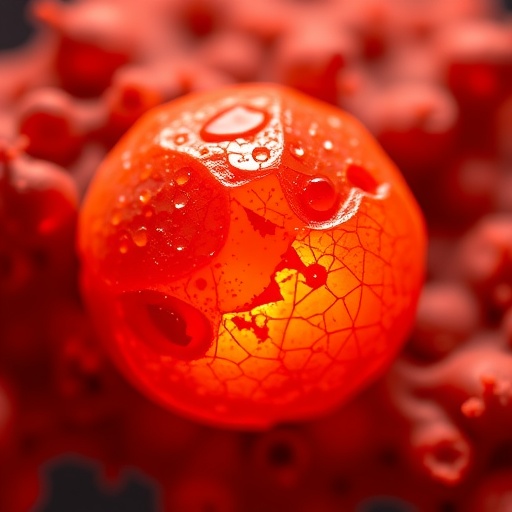
One of the most compelling applications of these 3D bioprinted melanoma models lies in their utility for assessing anticancer strategies that combine photodynamic therapy (PDT) with cutting-edge drug delivery systems. PDT, a treatment involving the activation of photosensitizers by specific wavelengths of light to produce cytotoxic reactive oxygen species, has shown potential against melanoma cells. However, its efficacy can be limited by challenges such as inadequate photosensitizer delivery and poor penetration of activating light into tumor tissues. Here, nanocarrier-based drug delivery systems meticulously engineered for targeted and controlled release come into play, optimizing the therapeutic payload delivered to tumor sites while minimizing off-target effects.
The synergy between PDT and advanced drug delivery vehicles can be methodically explored using 3D bioprinted models that recreate the tumor microenvironment, including barriers to drug and light penetration. This represents a significant leap over conventional culture systems, where the lack of realistic skin architecture hinders accurate prediction of therapeutic outcomes. Moreover, the tunable nature of bioprinting permits the fabrication of melanoma constructs with varying degrees of complexity and cell composition, thereby facilitating the screening of personalized treatment regimens and the examination of tumor heterogeneity.
Bioink formulation remains a crucial aspect of this field, demanding materials that support cell viability, encourage appropriate cell signaling, and replicate the mechanical properties of native skin. Researchers have been developing composite bioinks combining natural polymers such as collagen and hyaluronic acid with synthetic components to fine-tune printability and structural stability. These advancements permit the generation of melanoma models that not only survive the printing process but also exhibit functional characteristics like proliferation, migration, and invasion of melanoma cells within a matrix that simulates the skin extracellular matrix.
The dynamic interaction between melanoma cells and other skin-resident cells, such as fibroblasts, endothelial cells, and immune cells, can be faithfully studied within these bioprinted constructs. Recreating the intricate crosstalk and signaling within this microenvironment is critical for understanding treatment resistance mechanisms and tumor progression pathways. For example, incorporating endothelial cells can induce vascular mimicry, allowing researchers to evaluate how drug carriers and photosensitizers distribute within tumoral and peri-tumoral areas, thereby fine-tuning treatment parameters for maximal efficacy.
In addition to biological fidelity, 3D bioprinting streamlines reproducibility and scalability, which are essential for preclinical drug testing and regulatory approval processes. Unlike spontaneously formed spheroids or organoids, bioprinting provides consistent spatial cell patterning, ensuring that each sample is nearly identical in cellular composition and architecture. This reproducibility dramatically enhances the reliability of experimental results and enables high-throughput screening of drug candidates in complex tissue-like systems.
While this evolving technology is promising, challenges still remain, notably regarding the integration of fully functional immune components and the replication of the dynamic vascular networks observed in vivo. Future innovations might incorporate advanced biomaterials, vascularization techniques, and immune modulators to produce even more comprehensive melanoma models. Such advancements would provide an unparalleled platform for dissecting tumor immunology and for developing immunotherapeutic agents that complement PDT and nanocarrier-delivered drugs.
The combination of 3D bioprinted melanoma models with emerging therapeutic strategies underscores a paradigm shift in how anticancer drug screening and photodynamic therapy assessments are conducted. By bridging the gap between simplistic in vitro cultures and complex in vivo environments, these models promise to accelerate the pace of translational research, reduce reliance on animal testing, and ultimately improve clinical outcomes for patients with malignant melanoma.
In summary, the integration of bioprinting technology with melanoma research marks a formidable advance, offering robust platforms that recapitulate native skin conditions and tumor microenvironments with unprecedented precision. This enables a more insightful evaluation of contemporary anticancer strategies, combining photodynamic therapy with drug delivery systems tailored for superior targeting and efficacy. As these technologies mature, they have the potential to transform both experimental oncology and personalized medicine, providing new hope against one of the most lethal forms of skin cancer.
The ongoing evolution of melanoma modeling through 3D bioprinting invites a deeper exploration of tumor biology, therapeutic responsiveness, and drug delivery optimization. These advancements pave the way for definitive preclinical platforms that faithfully predict clinical outcomes, opening avenues for the development of novel combination therapies. Ultimately, the marriage of bioprinted skin constructs and state-of-the-art treatment modalities represents not only a technological breakthrough but also a beacon of hope in the fight against melanoma.
Subject of Research:
Article Title: 3D bioprinted melanoma models: a novel paradigm for the assessment of anticancer strategies combining PDT and drug delivery systems
Article References:
do Amaral, S.R., Atanasov, A.P., de Souza, D.C.M. et al. 3D bioprinted melanoma models: a novel paradigm for the assessment of anticancer strategies combining PDT and drug delivery systems. BioMed Eng OnLine 24, 132 (2025). https://doi.org/10.1186/s12938-025-01476-4
Image Credits: AI Generated
DOI: 10.1186/s12938-025-01476-4 (Published 06 November 2025)