In a groundbreaking study published in Nature, researchers have unveiled a pivotal vulnerability in lung adenocarcinoma (LUAD) tumors that could revolutionize cancer treatment strategies. FSP1, a protein previously understudied in the context of cancer progression, has emerged as an essential factor sustaining tumor growth in vivo, regardless of the diverse genetic drivers and co-mutations present in these malignancies. This discovery paves the way for the development of new targeted therapies that exploit ferroptosis, a unique form of iron-dependent cell death, to combat resistant lung cancers.
Lung adenocarcinoma represents a significant portion of lung cancer cases and often harbors a complex landscape of mutations involving genes such as KRAS, NRAS, EGFR, TP53, STK11, and KEAP1. These mutations contribute to tumor heterogeneity and therapeutic resistance, making it challenging to identify universal targets applicable across different genetic backgrounds. The study delves into the potential of targeting FSP1, a ferroptosis suppressor protein, as a common Achilles heel in these genetically diverse tumor types.
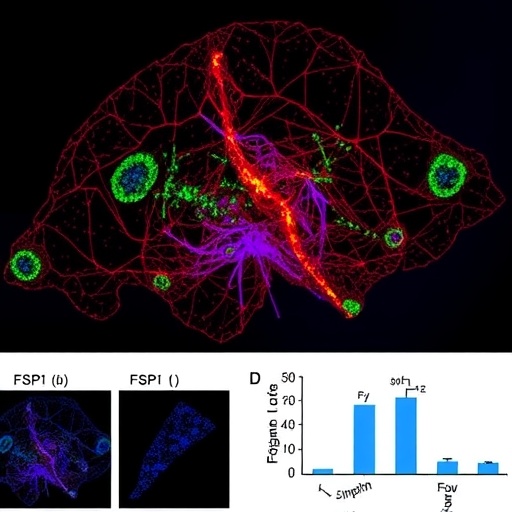
To ascertain the importance of FSP1 in tumorigenesis, the research team employed CRISPR-Cas9 technology to knock out the FSP1 gene in multiple human LUAD cell lines. These cell lines carried a broad spectrum of clinically relevant driver mutations, encompassing KRAS and TP53, NRAS and TP53, as well as EGFR and TP53 double mutants. Remarkably, FSP1 knockout consistently led to a marked decrease in tumor growth when these cells were implanted in murine models, revealing a pronounced dependence on FSP1 for in vivo tumor propagation.
Interestingly, despite the significant impact on tumor growth in living organisms, the removal of FSP1 did not impair the proliferation or survival of LUAD cells in standard in vitro conditions, unless exposed to ferroptosis-inducing agents like RSL3. This phenomenon highlights the complex tumor microenvironment’s role in modulating ferroptosis resistance mechanisms, which are absent in simplified culture conditions. It underscores the imperative for in vivo studies to capture the multifaceted biology underlying tumor survival.
Beyond commonly studied LUAD models, the dependency on FSP1 was also confirmed in tumors harboring mutations in the STK11 (LKB1) and KEAP1 genes, which are frequently associated with poor clinical outcomes. When FSP1 was ablated in LUAD cells possessing concurrent KRAS, KEAP1, and STK11 mutations, tumor growth was again profoundly suppressed in animal models. This reinforces the ubiquity of FSP1’s role across an array of molecularly distinct lung cancers and solidifies its position as a promising therapeutic target.
Expanding the scope of their investigation, the researchers turned their attention to pancreatic ductal adenocarcinoma (PDAC), characterized by similar KRAS and TP53 mutations that drive malignant progression. Deletion of FSP1 in PDAC cells similarly resulted in significant tumor growth inhibition in vivo, mirroring the lung cancer findings. This cross-lineage dependency suggests a broader biological principle where FSP1 is integral to tumor fitness beyond just lung cancers.
Mechanistically, FSP1 functions as a ferroptosis suppressor by preventing the accumulation of lethal lipid peroxides, which are normally detoxified to avert cell death. Tumor cells, notorious for their elevated oxidative stress and altered metabolism, rely heavily on FSP1 to sustain redox homeostasis and evade ferroptotic death signals. Targeting FSP1, therefore, disrupts this essential defense mechanism, sensitizing tumors to ferroptosis and hampering their expansion.
The translational potential of these findings is immense. Drugs designed to inhibit FSP1 could synergize with existing therapies to overcome resistance mechanisms that plague current treatment regimens, especially in tumors with poor prognosis driven by mutations in KRAS, STK11, or KEAP1. Importantly, the distinct discrepancy between in vitro and in vivo results advises that clinical development should consider the tumor microenvironment’s influence on therapeutic efficacy.
This study also challenges the traditional paradigm of cancer cell vulnerability assessment, emphasizing that dependencies witnessed in vivo may not always be recapitulated in cell culture. The tumor microenvironment—including immune cells, stromal interactions, and nutrient availability—likely contributes to FSP1’s critical role in promoting tumor fitness. Consequently, future research must integrate complex biological systems to better identify and validate novel targets like FSP1.
Moreover, the consistent requirement for FSP1 across diverse driver genotypes within LUAD and even extending into pancreatic cancer highlights a new, mutation-agnostic approach to targeting refractory solid tumors. Such strategies promise to broaden the applicability of precision medicine by focusing on convergent survival pathways essential to tumor maintenance rather than solely on individual oncogenic drivers.
The potential for ferroptosis induction as a therapeutic modality has garnered attention recently, yet effective agents remain limited. This work positions FSP1 inhibition as a prime candidate to unleash ferroptotic cell death selectively within tumors, offering a rescue from drug resistance and relapse. By triggering ferroptosis pharmacologically, clinicians could expand their arsenal against deadly cancers that have thus far evaded targeted therapies.
In summary, the discovery that FSP1 is essential for the growth of genetically diverse LUAD tumors, as well as KRAS-driven pancreatic tumors in vivo, unveils a vital metabolic vulnerability. Targeting this ferroptosis gatekeeper could transform the therapeutic landscape, offering new hope for patients with lung and potentially other solid tumors notorious for therapeutic resistance and poor survival.
These insights not only illuminate a critical survival mechanism exploited by aggressive cancers but also underscore the importance of integrated functional genomics and preclinical models in uncovering targetable tumor dependencies. As pharmaceutical efforts advance, FSP1 inhibitors may emerge as a cornerstone of next-generation ferroptosis-based cancer therapies.
Future studies will need to dissect the context-specific factors influencing FSP1 dependency and delineate combinatorial strategies that enhance ferroptotic vulnerability without affecting normal tissues. Nonetheless, the trajectory set by this landmark study heralds an exciting era in oncology where ferroptosis induction becomes a mainstay of precision cancer medicine.
Subject of Research: Functional requirement of FSP1 in tumor growth and its potential as a therapeutic target in lung adenocarcinoma and pancreatic ductal adenocarcinoma.
Article Title: Targeting FSP1 triggers ferroptosis in lung cancer.
Article References:
Wu, K., Vaughan, A.J., Bossowski, J.P. et al. Targeting FSP1 triggers ferroptosis in lung cancer. Nature (2025). https://doi.org/10.1038/s41586-025-09710-8
Image Credits: AI Generated