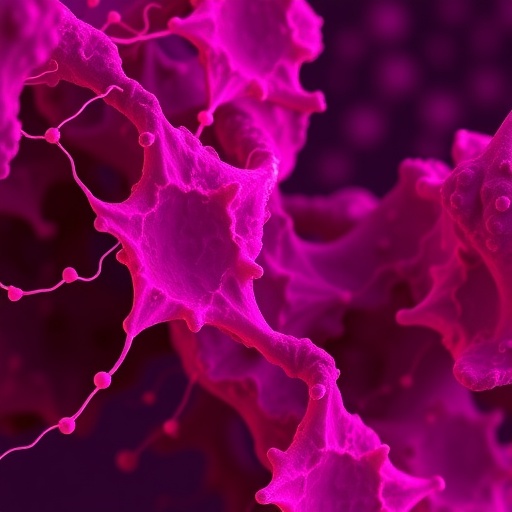
In the relentless battle against glioblastoma, one of the most aggressive and treatment-resistant forms of brain cancer, new research is shedding light on a cellular structure that might hold the key to future therapeutic strategies. Scientists have focused their attention on tunneling nanotubes (TNTs), tiny membranous channels that create direct cytoplasmic bridges between cells, facilitating rapid and efficient intercellular communication. These structures enable malignant cells to coordinate their activities, share resources, and resist therapeutic assaults more effectively, thereby complicating treatment efforts.
Glioblastoma’s notorious resilience and its ability to infiltrate surrounding brain tissue have long challenged oncologists. The research, published in the prestigious journal BMC Cancer, delves into how TNTs contribute to this malignancy’s adaptive mechanisms. Using the U87 MG glioblastoma cell line, the study explores how different chemotherapeutic agents and a potent cytoskeletal disruptor influence the formation and stability of these membrane nanotubes. Understanding the interplay between therapeutic agents and TNT networks offers potential pathways to dismantle the cellular communication system that tumors exploit.
Central to the investigation is the cytoskeleton—a dynamic scaffold within cells composed primarily of actin filaments and microtubules. This internal framework not only maintains cell shape but also underpins the formation and maintenance of structures like TNTs. Given this, the research team zeroed in on the role of actin and tubulin in TNT stability. Their experiments revealed that actin polymerization is crucial for TNT formation, whereas tubulin does not appear to have a significant stabilizing role in these structures.
The study employed cytochalasin B (CytoB), a well-known inhibitor of actin polymerization, to test its impact on TNT networks within U87 MG cells. Remarkably, CytoB treatment led to a significant reduction in the number of TNTs, corroborating the hypothesis that actin dynamics are essential for the development and persistence of these nanotubes. This finding underscores actin’s fundamental role in the structural integrity and functionality of intercellular conduits.
Conversely, the research also assessed the effects of chemotherapeutic drugs temozolomide (TMZ) and cytarabine (AraC), both used in various cancer treatment regimens. The expectation was that these drugs, known to interfere with DNA synthesis and cell cycle progression, might also disrupt TNT networks as part of their anti-cancer activity. However, the results revealed an unanticipated resilience of TNTs; neither TMZ nor AraC significantly diminished the number or integrity of TNTs, nor did they alter the actin composition within these specialized structures.
This resilience of TNTs in the face of conventional chemotherapy poses a formidable obstacle to effective glioblastoma management. TNT-mediated communication pathways likely provide a protective niche for tumor cells, enabling them to share survival signals and molecular cargo that help circumvent the cytotoxic effects of drugs. Consequently, current treatments may inadvertently overlook these cellular lifelines that facilitate therapy resistance.
The implications of these findings are profound. They suggest that therapeutic strategies targeting TNT formation and maintenance could enhance the efficacy of existing chemotherapeutic agents. Disrupting the actin cytoskeletal framework crucial for TNT stability represents a promising avenue to impede the tumor’s cellular networking capabilities. By crippling these communication pathways, cancer cells may become more vulnerable to cytotoxic insults.
Moreover, the study emphasizes the necessity for a paradigm shift in glioblastoma therapy research. While DNA-damaging agents like TMZ and AraC remain staples in clinical practice, their inability to suppress TNT-mediated cellular collaboration signals a significant gap in treatment design. Future drug development should incorporate agents capable of disrupting TNT dynamics, potentially in combination with standard chemotherapies to achieve synergistic effects.
At a molecular level, understanding how TNTs facilitate the exchange of oncogenic signals, organelles, and resistance factors between glioblastoma cells could reveal novel biomarkers and therapeutic targets. Detailed characterization of TNT composition and formation mechanisms may pave the way for innovative treatments that selectively dismantle tumor networking without harming innocent bystander cells.
The investigation into TNTs also opens broader questions about the tumor microenvironment. Intercellular communication is not just a cancer cell property but a vital component of tissue homeostasis and immune regulation. Therefore, any approaches aimed at TNT disruption must carefully balance therapeutic benefits against potential impacts on healthy cellular interactions within the brain.
Another intriguing dimension of this research is the role of TNTs in facilitating tumor cell invasion and metastasis. By creating expansive cellular networks, glioblastoma cells can coordinate strategies to infiltrate surrounding tissues, evade immune detection, and migrate to inaccessible regions. Consequently, targeting TNTs might also impede tumor spread and improve surgical outcomes by containing tumor cell dissemination.
The adaptation of tumor cells through TNT-mediated communication resonates with the larger theme of cancer as a complex, heterogeneous ecosystem. Therapeutic resistance often arises not merely from genetic mutations but from dynamic intercellular interactions that promote collective survival. As such, anticancer strategies must evolve beyond targeting individual cells to disrupting cell-to-cell cooperation networks.
This study underscores the urgent need for multidisciplinary approaches that combine molecular biology, pharmacology, and bioengineering to develop TNT-specific inhibitors. Compounds like cytochalasin B, despite their potent actin-disrupting properties, have limitations and toxicity concerns that preclude their clinical use. The discovery or design of more selective and safer agents will be critical to translating these findings into viable treatments.
In summary, the research reveals that TNTs in glioblastoma cells represent a robust intercellular network essential for tumor survival and adaptability. The selective vulnerability of these structures to actin polymerization inhibition, juxtaposed with their resistance to chemotherapy, highlights a crucial therapeutic target. Moving forward, integrating TNT-targeted therapies could revolutionize glioblastoma treatment paradigms, offering new hope against this formidable disease.
As researchers continue to unravel the complexities of cellular communication in cancer, the role of tunneling nanotubes emerges as a pivotal frontier. By illuminating the structural and functional underpinnings of these tiny conduits, the scientific community moves closer to dismantling the cellular alliances that empower tumors. This study propels the field toward innovative, more effective interventions, underscoring the promise of targeting the microarchitectural fabric of tumor cell communication.
Subject of Research: Effect of chemotherapeutic drugs and cytochalasin B on tunneling nanotubes in U87 MG glioblastoma cells
Article Title: Effect of chemotherapeutic drugs and cytochalasin B on tunneling nanotubes in U87 MG cells
Article References:
Matejka, N., Neubauer, J. & Reindl, J. Effect of chemotherapeutic drugs and cytochalasin B on tunneling nanotubes in U87 MG cells. BMC Cancer 25, 1709 (2025). https://doi.org/10.1186/s12885-025-15204-7
Image Credits: Scienmag.com
DOI: 10.1186/s12885-025-15204-7
Keywords: glioblastoma, tunneling nanotubes, TNTs, U87 MG cells, actin polymerization, cytochalasin B, temozolomide, cytarabine, chemotherapy resistance, cytoskeleton, intercellular communication