In a groundbreaking study published in BMC Psychiatry, researchers have provided valuable insights into the long-term effects of assertive community treatment (ACT) for individuals with severe mental disorders in Japan. This comprehensive 7-year follow-up of a randomized controlled trial (RCT) sheds light on the enduring benefits of ACT programs compared to treatment-as-usual (TAU) in reducing hospitalization frequency, a crucial metric in mental health care management.
ACT, recognized worldwide as an intensive, community-based intervention, targets individuals facing persistent and severe psychiatric conditions. Traditionally, ACT involves a multidisciplinary team approach aimed at minimizing hospital readmissions and promoting independence in community living. Despite its widespread use, data on the sustained impact of ACT over extended periods have been conspicuously sparse. This landmark study addresses that gap by meticulously tracking patient outcomes seven years after initial treatment allocation.
The investigation revisited participants from a prior RCT conducted in Japan, where ACT’s short-term efficacy was initially evaluated. Researchers revisited medical records of 63 participants—34 in the ACT group and 29 receiving TAU—offering an unprecedented longitudinal perspective. Readmission incidences, frequency, and the cumulative duration of hospital stays were key parameters to evaluate the relative success of both treatment modalities over this extended timeline.
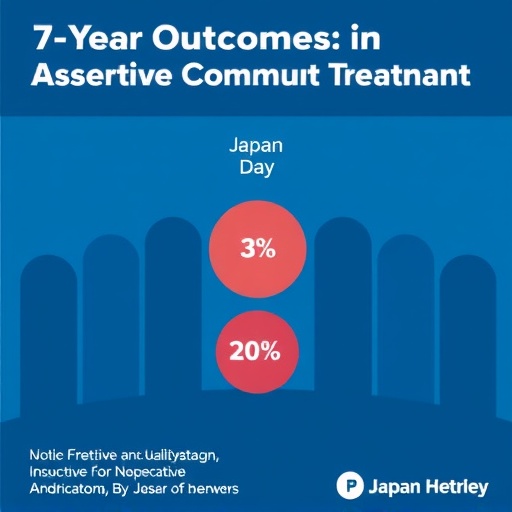
Results revealed a nuanced but compelling advantage of ACT in reducing hospital readmission frequency. While the overall readmission rates between TAU (79%) and ACT (53%) groups did not reach statistical significance, the ACT cohort experienced significantly fewer hospitalizations (p = 0.030), underscoring ACT’s role in diminishing the episodic return to inpatient care. Importantly, this effect became markedly pronounced approximately two years post-randomization, suggesting a delayed but sustained therapeutic benefit.
Contrary to expectations, cumulative days of hospitalization did not significantly differ between the groups. This insight suggests that while ACT may reduce the number of re-hospitalizations, the length of each stay when hospitalization occurs might remain consistent with standard care approaches. The complexity of factors influencing hospitalization length, including clinical severity and social determinants, merits deeper exploration in future studies to optimize ACT protocols.
This Japanese RCT follow-up provides crucial empirical evidence endorsing ACT’s capacity to modulate the chronic course of severe mental illness through long-term community-based intervention. The findings imply that ACT’s intensive engagement strategies, continuous monitoring, and personalized care plans cumulatively yield fewer relapse episodes necessitating hospitalization, enhancing patient stability in the home environment.
The timing of the observed benefits is particularly intriguing. Researchers postulate that the initial years of receiving ACT are likely critical for building trust, deploying adaptive treatment plans, and enabling gradual behavioral and symptomatic improvement. The delayed manifestation of reduced hospitalization frequency aligns with the expected trajectory of complex psychiatric rehabilitation, which often requires sustained intervention to translate into durable outcomes.
Despite its promising results, the study’s scope is limited to the Japanese healthcare context, characterized by unique medical, cultural, and social nuances. Therefore, extrapolation to other countries demands cautious interpretation. Replicating such comprehensive longitudinal studies across different healthcare systems will be instrumental in delineating how varying community resources, policy frameworks, and cultural attitudes influence long-term ACT efficacy.
Moreover, the retrospective registration of this trial in 2025 signifies a call to action for future studies to employ prospective designs with pre-registered protocols to enhance methodological transparency and reproducibility. Addressing this rigor will further consolidate ACT’s evidence base and expedite its global advocacy as a cornerstone of community mental health care.
The implications for clinical practice and health policy are profound. By demonstrating a statistically significant reduction in hospital readmissions over seven years, this study supports sustained investment and expansion of ACT services. Policymakers and healthcare providers might consider adopting or scaling ACT frameworks to alleviate hospital burden, improve patient quality of life, and optimize resource allocation in mental health systems.
In sum, this seminal 7-year follow-up study enriches the scientific discourse on assertive community treatment, reinforcing its value as a long-term strategy for managing severe mental illness. The research addresses a pivotal knowledge gap, offering a roadmap for integrating intensive community care programs that yield lasting improvements in patient outcomes and foster societal inclusion.
Future investigations should focus on mechanistic insights into which components of ACT drive its enduring benefits, explore patient-centered outcomes beyond hospitalization metrics, and refine intervention timing to maximize therapeutic impact. The intersection of clinical innovation, health services research, and cultural adaptation promises to unlock the full potential of ACT worldwide.
As mental health challenges continue to impose substantial individual and societal burdens, this evidence positions assertive community treatment at the forefront of sustainable solutions. Patients, clinicians, and policymakers alike stand to gain from embracing ACT’s demonstrated capacity to curtail hospitalization frequency, thereby transforming lives through community-centric psychiatric care.
Subject of Research: Long-term effects of assertive community treatment (ACT) on hospitalization outcomes in individuals with severe mental illness.
Article Title: Long-term outcomes of assertive community treatment in Japan: 7-year follow-up of a randomized controlled trial.
Article References:
Satake, N., Yamaguchi, S., Sato, S. et al. Long-term outcomes of assertive community treatment in Japan: 7-year follow-up of a randomized controlled trial. BMC Psychiatry 25, 870 (2025). https://doi.org/10.1186/s12888-025-07311-3
Image Credits: AI Generated