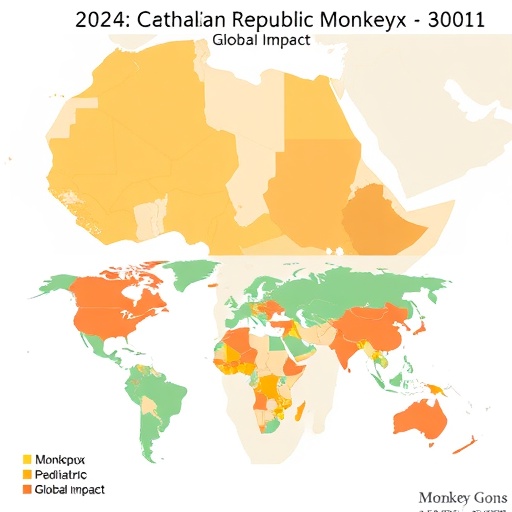
In 2024, the Central African Republic (CAR) became the epicenter of an unprecedented outbreak of the monkeypox virus (MPXV), signaling a striking transformation in the epidemiology of this once-neglected zoonotic disease. Historically confined to children within endemic regions, this outbreak, designated MPXV-CAR-2024, reveals a significant shift in both the demographic profile of those infected and the underlying modes of transmission. Unlike previous episodes, where the virus spread predominantly through close household contacts and animal reservoirs, the current outbreak demonstrates a marked rise in adult cases, notably among men who have sex with men (MSM), underscoring the sexual transmission pathway as a dominant driver.
This epidemiological shift challenges the longstanding paradigm that viewed monkeypox primarily as a pediatric concern, expanding its relevance to wider, more sexually active populations in urban centers. The virus itself, a member of the Orthopoxvirus genus, remains genetically consistent with clade I strains historically reported in Central Africa, but the social and behavioral context of its propagation has evolved. Intensive contact tracing and phylogenetic analyses confirm the emergence of sexual networks as epicenters, where sustained human-to-human transmission now occurs outside traditional zoonotic spillover events.
Clinically, monkeypox manifests with a characteristic prodrome of fever, malaise, lymphadenopathy, and a subsequent vesiculopustular rash. Pediatric patients have historically experienced more severe clinical courses, with complications such as secondary bacterial infections, pneumonia, and rare instances of encephalitis contributing to increased morbidity. In the MPXV-CAR-2024 outbreak, these severe pediatric presentations have persisted, compounded by limited access to comprehensive healthcare in resource-poor settings. Severely affected children often require advanced medical interventions, which are scarce within the overwhelmed healthcare facilities of CAR.
Beyond clinical complexities, the outbreak has exerted immense pressure on the pediatric healthcare infrastructure, revealing systemic vulnerabilities. Hospitals and clinics are strained by surging patient loads, depletion of critical medical supplies, and the challenge of safely isolating contagious individuals. Additionally, healthcare workers confront elevated occupational risks due to insufficient personal protective equipment (PPE) and inadequate infection prevention control protocols, escalating the potential for nosocomial transmission. These factors combine to destabilize routine healthcare services, resulting in broader public health implications, including interruptions in vaccination programs and essential child health services.
The role of antiviral therapies and vaccines in managing mpox remains pivotal, yet accessibility is severely constrained in CAR and similar low-resource environments. The attenuated smallpox vaccines and newer antivirals such as tecovirimat have demonstrated efficacy in clinical trials, curbing viral replication and mitigating disease severity. However, geopolitical disparities in pharmaceutical availability perpetuate inequities, leaving the most vulnerable populations underserved. This inequity underscores an urgent need for an international framework to facilitate equitable distribution of medical countermeasures.
On a global scale, the MPXV-CAR-2024 outbreak reaffirms the necessity for vigilant surveillance augmented by sophisticated molecular diagnostics and genomic epidemiology. Enhanced case finding and rapid reporting mechanisms are critical to capturing real-time data, enabling public health authorities to mount timely interventions. Moreover, the outbreak has exposed gaps in public health communication, where misinformation and stigma—especially around the predominant transmission in MSM communities—hamper effective outreach and adherence to preventive measures.
Incorporating culturally sensitive public health messaging is thus indispensable. Efforts must focus on community engagement strategies that respect local norms and counteract discrimination while promoting sexual health education and the adoption of safer sexual practices. Training frontline health workers in these communication strategies is essential to build trust and facilitate voluntary testing, isolation, and treatment adherence.
International cooperation emerges as the linchpin in curbing this outbreak and preempting future mpox epidemics. Multinational collaborations must prioritize resource mobilization, knowledge exchange, and capacity building within endemic regions. The current crisis offers a clarion call to integrate mpox more comprehensively into global health security agendas, benefiting from lessons learned during recent pandemics such as COVID-19, which underscored the value of coordinated responses and robust supply chains.
From a virological perspective, ongoing genomic surveillance has not demonstrated significant mutations in MPXV-CAR-2024 that would suggest increased viral fitness or pathogenicity. This finding contrasts with initial concerns about potential viral adaptation toward enhanced human transmissibility. Nonetheless, the altered epidemiological landscape warrants continuous molecular monitoring to promptly detect any emergent variants that could impact transmissibility, clinical outcomes, or therapeutic susceptibility.
Moreover, the outbreak’s emphasis on adult sexual transmission networks raises pivotal questions about potential viral persistence and reservoirs within the human population. Research is underway to elucidate the dynamics of viral shedding and infectivity duration in genital secretions, vital for refining prevention strategies. These scientific inquiries are complemented by epidemiological studies assessing the social determinants that facilitate spread within marginalized populations, guiding tailored interventions.
The MPXV-CAR-2024 outbreak also underscores the intersectionality of biological and social vulnerabilities. Factors such as poverty, limited healthcare access, and social stigma coalesce, amplifying outbreak intensity and complicating containment. Addressing these determinants through a One Health approach —linking human health, animal health, and environmental factors—could deliver more sustainable control measures, especially given the zoonotic origins of monkeypox.
As the outbreak progresses, the importance of integrated, real-time data analytics cannot be overstated. Leveraging digital health technologies—including mobile reporting apps and AI-driven predictive models—can enhance outbreak forecasting and resource allocation. These innovations promise to transform the response paradigm from reactive to proactive, minimizing future transmission and health system disruptions.
In the public health domain, vaccination campaigns tailored to at-risk populations, including MSM and healthcare workers, are critical. The introduction of next-generation vaccines with improved safety profiles and longer-lasting immunity would be a significant advancement. Additionally, strategic stockpiling and distribution mechanisms must be instituted globally to ensure timely availability during emergent mpox flare-ups.
Equipping healthcare workers through comprehensive training programs focused on mpox recognition, patient management, and biosafety protocols is paramount. This education must extend to psychosocial support frameworks that shield frontline workers from burnout and stress, which have intensified amid the protracted outbreak.
Lastly, the MPXV-CAR-2024 outbreak serves as a potent reminder of the need for heightened global preparedness against emerging infectious diseases. It highlights how shifting epidemiological landscapes can alter the trajectory and burden of once-neglected illnesses, demanding adaptive, multifaceted responses. Strengthening health system resilience, fostering international solidarity, and investing in cutting-edge research are indispensable to curtailing not only monkeypox but future pandemics.
Subject of Research: The epidemiological evolution, clinical characteristics, public health impact, and global health implications of the 2024 monkeypox outbreak in the Central African Republic, with an emphasis on pediatric involvement and transmission dynamics.
Article Title: The 2024 Central African Republic monkeypox outbreak: implications for pediatric involvement and global health.
Article References:
Mohamed, M.G., Islam, M.R. The 2024 Central African Republic monkeypox outbreak: implications for pediatric involvement and global health.
Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04461-8
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41390-025-04461-8