In the evolving realm of reproductive medicine, oocyte cryopreservation techniques have witnessed significant advancements, positioning themselves as viable options for various fertility preservation strategies. The recent comparative analysis conducted by Liu et al. and published in the Journal of Ovarian Research reveals that oocyte cryopreservation through controlled ovarian stimulation (COS) presents distinct advantages over in vitro maturation (IVM) techniques when observed over a prolonged period of up to 12 years. This extensive study not only underscores the efficacy of these methods but also provides critical insights for clinicians and patients alike, navigating the complex landscape of fertility preservation.
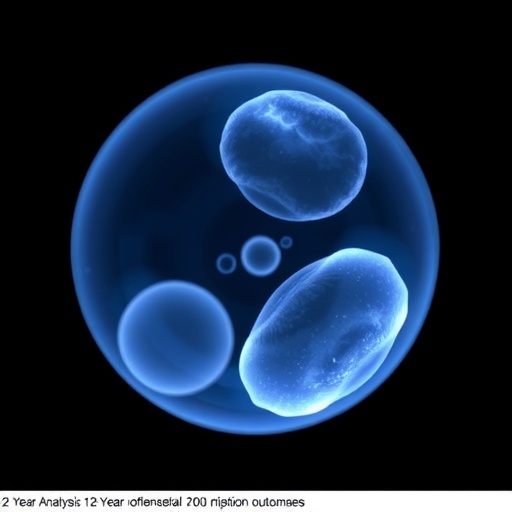
Oocyte cryopreservation, the process of freezing and storing oocytes for future use, has become increasingly popular among women seeking to delay childbirth for personal or medical reasons. Historically, the effectiveness of this procedure has been closely related to the maturation and developmental potential of the oocytes recovered, prompting ongoing research into optimizing techniques to enhance success rates. Liu and colleagues’ study encapsulates a comprehensive review of outcomes derived from two prevalent methodologies: controlled ovarian stimulation, where hormonal treatments yield mature oocytes, and in vitro maturation, an innovative strategy attempting to mature oocytes in the laboratory setting.
The overarchingly positive findings from the analysis reveal that oocytes harvested via controlled ovarian stimulation tend to exhibit higher fertilization rates, leading to increased embryo viability when compared to those recruited through in vitro maturation techniques. This assertion is particularly significant in the context of advancing assisted reproductive technologies (ART) and the necessity for high-quality oocytes to maximize the chances of implantation and successful pregnancies.
Delving deeper into the statistics, the longitudinal aspect of the study spans an impressive 12 years, allowing the researchers to compile extensive data indicative of the long-term applicability and success of different cryopreservation strategies. Their findings suggest that while IVM offers a less invasive route and may appeal to patients wary of hormonal stimulation, the resultant maturity and quality of oocytes are paramount for enhancing pregnancy rates in ART.
Moreover, the research conducted by Liu et al. reveals a compelling narrative surrounding the socioeconomic factors influencing the choice of oocyte preservation methods. For instance, in regions where resources are limited, IVM may present a cost-effective alternative; however, the necessity of recognizing its limitations is critical. The higher success rates associated with COS indicate that the initial financial outlay may pale in comparison to the long-term implications of higher pregnancy rates and successful live births associated with mature oocytes.
Interestingly, the analysis also touches upon the psychological dimensions of fertility preservation. Patients often experience stress and anxiety surrounding their reproductive choices, particularly when facing medical conditions or age-related declines in fertility. Understanding the potential differences in outcomes associated with various cryopreservation techniques serves not only to inform clinical decision-making but also to provide emotional reassurance to patients as they navigate these profound life choices.
As the study emphasizes the disparity in outcomes between the two methodologies, it also advocates for the unification of clinical practices with a keen awareness of the long-term consequences. Fertility specialists and reproductive endocrinologists must take these findings to heart, integrating evidence-based practices into their patient care strategies to ensure optimal outcomes.
The implications of Liu et al.’s analysis extend beyond mere statistical fascination; it urges a broader conversation about reproductive rights and accessibility to state-of-the-art fertility treatments. As more women seek to exercise autonomy over their reproductive health, understanding which methods yield the most favorable outcomes is paramount in shaping future policies and funding for reproductive technologies.
In summary, the comparative analysis presented by Liu et al. is not merely a reflection on the technical specifications of oocyte cryopreservation techniques; it represents a clarion call for ongoing research and discussions within reproductive medicine. As the study sheds light on which methodologies are more advantageous, it provides a foundation for advocating best practices that align with the evolving needs and expectations of patients seeking fertility preservation.
As this research landscape continues to evolve, it will be crucial for clinicians and patients alike to remain aware of new findings and technologies that could further enhance oocyte preservation outcomes. The future of reproductive medicine is bright, and as we leverage such insights, we gain further capacity to support the aspirations and hope of individuals wishing to conceive.
In conclusion, Liu et al. have contributed significantly to the body of evidence supporting controlled ovarian stimulation as a superior method for oocyte cryopreservation, pushing the boundaries of what is known and expected within the field. The study not only illuminates the path forward for clinical practices but also enriches the broader dialogue surrounding fertility preservation and reproductive health initiatives. As we reflect on these advancements, we are reminded of the profound and lasting impact such innovations have on individual lives and society at large.
Subject of Research: Oocyte Cryopreservation Techniques
Article Title: Clinical outcomes over 12 years: a comparative analysis of oocyte cryopreservation from controlled ovarian stimulation and in vitro maturation retrieved from ovarian tissue.
Article References: Liu, X., Zhao, W., Sun, P. et al. Clinical outcomes over 12 years: a comparative analysis of oocyte cryopreservation from controlled ovarian stimulation and in vitro maturation retrieved from ovarian tissue. J Ovarian Res 18, 241 (2025). https://doi.org/10.1186/s13048-025-01847-4
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s13048-025-01847-4
Keywords: Oocyte cryopreservation, Controlled ovarian stimulation, In vitro maturation, Assisted reproductive technology, Fertility preservation, Long-term outcomes, Reproductive medicine, Patient care.