The Department of Defense awarded a little more than $1.9 million to a multidisciplinary team of researchers at the University of Arkansas and University of Arkansas for Medical Sciences to develop a wearable device that will assist with the early detection and monitoring of internal and external bleeding. The grant comes as part of the Department of Defense’s prestigious Congressionally Directed Medical Research Programs.

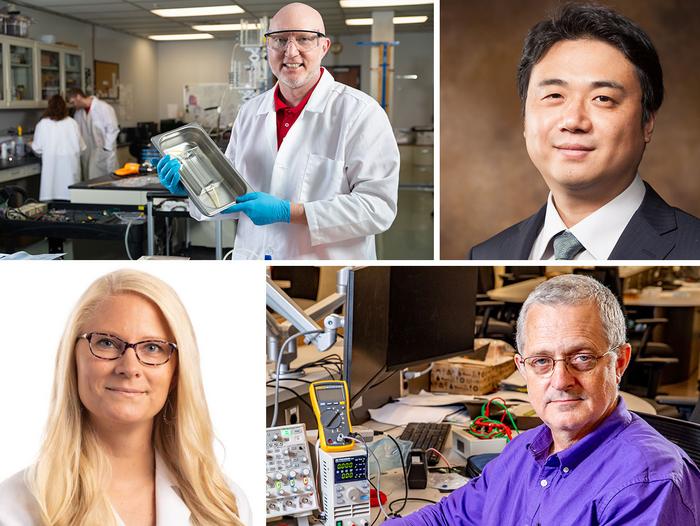
Credit: University Relations
The Department of Defense awarded a little more than $1.9 million to a multidisciplinary team of researchers at the University of Arkansas and University of Arkansas for Medical Sciences to develop a wearable device that will assist with the early detection and monitoring of internal and external bleeding. The grant comes as part of the Department of Defense’s prestigious Congressionally Directed Medical Research Programs.
Hemorrhagic shock is currently the leading cause of preventable death in casualty care settings. Existing methods often fail to detect blood loss until the onset of shock, which can be too late for some patients. This makes early detection and management of bleeding-related conditions critical to improving survival rates.
The team is designing a mobile device that can detect blood pressure waveforms, which correlate with the volume of blood within the blood vessels, the “intravascular volume,” and can be used to determine if blood volume is falling due to hemorrhaging. This will enable first responders and hospital staff to get more accurate readings earlier and respond with better timed and more precisely calibrated care.
The principal investigator on the four-year award is associate professor of biomedical engineering at the U of A, Morten Jensen, who also has a background in electrical and computer engineering and has worked in industry with sensor and signal analysis technologies. Jensen will be joined by Jingxian Wu, a U of A professor of electrical engineering, and Robert Saunders, an associate department head of electrical engineering and computer science. Hanna Jensen, an assistant professor in the Department of Surgery at UAMS and course director of the school’s cardiovascular module, will oversee the translational and clinical phases of the project.
The proposed work will have three goals. First, the team will develop machine learning models and algorithms to analyze the pressure signals for blood loss detection. This involves optimizing learning algorithms with a small amount of data, developing real-time software and creating models based on physiological data. This will improve patient care by enabling accurate and efficient detection of blood loss.
Second, they will prototype and develop a cost-effective wearable device for detecting blood loss. Finally, the team will test the device through clinical trials in a wearable configuration. The goal is to create a device that functions optimally, meets design parameters and performs accurately and reliably in real-world scenarios.
Morten Jensen, who is a native of Denmark, said, “Our similar educational backgrounds make it very exciting to collaborate with Jingxian Wu and Robert Saunders. I also served in the Danish military and know first-hand the importance of reliable equipment that works fast and is lightweight.”
Saunders, who is a first responder in Madison County with the volunteer fire department, will be tasked with constructing, and then shrinking down, the prototype. He noted that the device would be extremely useful when medics showed up to an incident with multiple casualties and a limited amount of saline (in Madison County, casualties may be as many as 20 minutes from the nearest hospital). The device would help first responders determine exactly who needs the fluid and how badly, optimizing the use of limited resources. The device would also remain attached to anyone involved in the incident in the event their blood pressure suddenly crashed due to a delayed reaction — at which point, fluids could be immediately administered.
Ultimately, the team’s goal is to develop a device that is less than an inch square and sells for less than $100. It would have a catheter that connects to a vein as well as a port to which an IV bag could be connected.